WHAT YOU SHOULD KNOW ABOUT GLAUCOMA: FACTS AND MYTHS
Myths:
People With Perfect Vision Cannot Develop Glaucoma
There Is Nothing You Can Do Once You Have Glaucoma
Other Myths and Misconceptions
Glaucoma is a medical condition when the individual suffers from damage to the eye’s optic nerve. This damage is often the result of abnormally high pressure in the eye. Glaucoma is one of the leading causes of blindness for people over the age of 50 but can affect all age groups [1].
There are a lot of myths about glaucoma. In this article we will look at some of the common ones.
MYTH: Glaucoma Has Obvious Symptoms
Fact: Glaucoma is commonly known as the "silent thief of sight" because, in its early stages, it usually does not exhibit any symptoms. This is especially true of acute angle closure glaucoma, the most common type. Many patients who have acute angle closure glaucoma do not notice their symptoms until it is too late and they are already suffering from vision loss. This can make glaucoma especially difficult to detect unless a patient seeks a regular eye examination.
In moderate to severe cases, symptoms of glaucoma can include blurred vision, severe pain in the eye and head, and nausea. If detected early on, a doctor can prescribe medication to protect against loss of vision. The risk of glaucoma increases with age. A patient has a higher chance of a successful treatment during their younger years.
Glaucoma should be treated as soon as possible. Some symptoms remain dormant in the early stages. Ignoring glaucoma until the condition becomes more severe can make treatment more complicated and lead to severe symptoms. Treatment can be effective in the early stages of glaucoma and prevent further damage.
MYTH: Glaucoma Only Affects One Eye
Fact: Glaucoma usually affects both eyes. However, glaucoma can be worse in one eye. If left untreated, glaucoma can spread from one eye to the other. The reality is that glaucoma is a progressive condition and does not affect both eyes at the same rate in most cases. It may take 5 to 10 years for glaucoma to affect the other eye.
It is currently not known why each eye is affected differently by glaucoma. Research points to genetics as a primary factor[2]. In rare cases, a surgical correction in one eye can trigger symptoms of glaucoma in another eye. Events like this still need further investigation to understand the underlying causes.
MYTH: People With Perfect Vision Cannot Develop Glaucoma
Fact: Glaucoma can be hereditary or become activated later in life. The observation that glaucoma can occur in people with 20/20 vision is taken from clinical studies. These studies are usually performed in patients who are able to detect glaucoma in the early stages.
People with 20/20 vision who develop glaucoma in one eye may retain 20/20 vision in the unaffected eye. If treatment is taken soon enough, the effects of glaucoma can be mitigated and localized to only one eye. Avoiding long exposure to bright lights and other harmful stimuli to the eyes can lower the chances of advanced progression.
MYTH: There Is Nothing You Can Do Once You Have Glaucoma
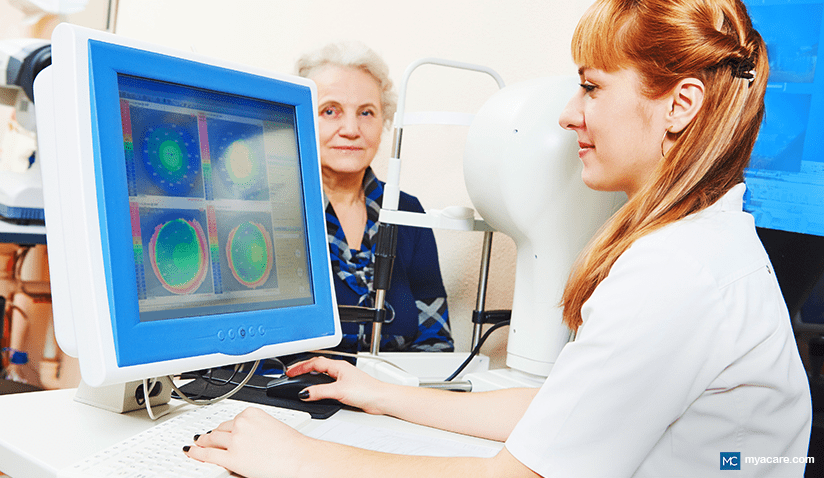
Fact: Currently, there is no cure for glaucoma. However, glaucoma can be treated with eye drops, medication, laser treatment, or surgery.[3] A doctor can diagnose an individual through a series of measurements and tests. Doctors generally check for intraocular pressure, damage to the optic nerve, corneal thickness, and a few other factors. Patients are scheduled for regular checkups to prevent further vision loss.
Prescription medications such as eye drops include biological inhibitors and agonists that improve the flow of liquid to the eye. More severe symptoms of glaucoma may require surgery. Unlike medication, surgery quickly drains excess fluid from the eye to relieve pressure. Some common surgeries include laser therapy and minimally invasive glaucoma surgery (MIGS).
The best way to prevent glaucoma is to go for regular eye exams. There are many non-invasive procedures that a doctor can offer a patient during the early stages. An ophthalmologist can offer proper guidance for deciding which is the best treatment.
Other Myths and Misconceptions
Myth: All Patients With Glaucoma Have Higher Intraocular Pressure (IOP)
Fact: While high intraocular pressure (IOP) is a common risk factor for glaucoma, it is not true that all patients with glaucoma have elevated IOP.
Some individuals may have normal or even low IOP and still develop glaucoma. Glaucoma is a complex disease that involves various factors, including optic nerve damage and visual field loss, in addition to IOP. It is crucial to keep in mind that, even in the absence of a high IOP, routine eye exams and screenings are required to identify glaucoma.
Myth: Glaucoma Only Affects Old People
Fact: Although glaucoma is the most common cause of blindness in the elderly, it can afflict individuals of all ages, including young adults and infants. It is common for glaucoma symptoms to begin affecting one during their 40s and to progress over the course of 5-10 years.
Myth: If Left Untreated, Cataract Turns Into Glaucoma
Fact: Cataracts and glaucoma are two different eye conditions, and cataracts do not progress into glaucoma. Blurred vision is caused by cataracts, which arise when the eye's lens gets clouded. Conversely, glaucoma is an illness that harms the optic nerve and, if unchecked, can cause blindness.
While both cataracts and glaucoma can occur simultaneously in some individuals, cataracts do not progress into glaucoma. To effectively manage and cure these diseases, it is crucial to have appropriate medical attention as well as routine eye exams.
Myth: Glaucoma Frequently Causes Eye Pain
Fact: Eye pain is not a common symptom for most types of glaucoma. In fact, the only symptom glaucoma is known for is vision loss, which is not even noticeable until the later stages of the condition.
It is important to note that while glaucoma may not typically cause eye pain, there are certain types of glaucoma, such as acute angle-closure glaucoma, that can cause sudden eye pain, redness, and blurred vision. This type of glaucoma is less common and constitutes a medical emergency. If your eyes suddenly begin to ache with blurred vision, you ought to seek medical attention immediately.
Myth: An Increased Risk of Glaucoma Is Associated With Prolonged Computer Screen Time
Fact: There is no scientific evidence to support the claim that spending too much time looking at a computer screen raises the risk of glaucoma. Glaucoma is primarily caused by factors such as high intraocular pressure, genetics, age, and certain medical conditions.
Eye strain and discomfort, also known as computer vision syndrome[4], can result from prolonged computer use. It primarily affects the ciliary muscles, which control the shape of the lens, and the extraocular muscles, which control eye movements, resulting in symptoms such as dryness, blurred vision, headaches, and eye fatigue.
Glaucoma is an eye disease in which progressive damage to the optic nerve leads to blindness. The optic nerve is responsible for carrying visual information from the eye to the brain. Eye strain from computer use does not cause damage to the optic nerve, yet it can increase the risk for other visual problems, such as myopia or nearsightedness. In those already suffering from myopia, computer vision syndrome may increase glaucoma risk, as severe or high myopia is linked to glaucoma risk.
It is advised to adhere to the 20-20-20 rule, which states that you should look away from your screen for 20 seconds every 20 minutes and concentrate on something that is at least 20 feet away in order to lessen the chance of eye strain. Additionally, it is important to take regular breaks, adjust the lighting and glare on the screen, and ensure that the computer screen is positioned at a comfortable distance and angle.
Myth: Surgery Can Cure Glaucoma
Fact: There is no cure for glaucoma. Surgery for glaucoma can help lower intraocular pressure and slow down the progression of glaucoma.
Different types of eye surgery for glaucoma include trabeculectomy [5], glaucoma drainage device implants, and laser trabeculoplasty.
- Trabeculectomy involves opening a new drainage route for the eye to reduce intraocular pressure.
- Glaucoma drainage devices are small implants that help drain excess fluid from the eye.
- Laser trabeculoplasty uses a laser to improve the drainage of fluid in the eye.
These surgeries aim to lower intraocular pressure and manage glaucoma. It is important to speak with an eye care specialist to figure out which course of action is best for your particular situation.
Myth: Testing for Glaucoma Is Painful
Fact: Testing for glaucoma is not typically painful. The process of diagnosing and screening for glaucoma involves a number of tests to assess the condition of the eyes and detect any signs of the disease. While some of the tests may cause temporary discomfort, most of them are non-invasive and painless.
The tonometry test, which gauges intraocular pressure, is the most widely used diagnostic procedure for glaucoma. This test involves a quick puff of air onto the surface of the eye or the use of a small instrument to gently touch the eye. While it may feel slightly uncomfortable or cause a brief sensation, it is generally not painful.[6]
Other tests for glaucoma may include
- Gonioscopy (eye drainage assessment) is used to evaluate the drainage angle of the eye, which can be affected in certain types of glaucoma.
- Ophthalmoscopy (optic nerve examination) allows an eye care professional to examine the optic nerve, retina, and blood vessels in the eye for any signs of damage or abnormalities.
- Visual field testing assesses how well the patient sees out of the corners of their eyes and checks for any loss of peripheral vision.
These tests are also painless and only require the patient to sit still and follow the instructions given by the eye care professional.
Myth: Glaucoma Is Inherited, and Since No One In My Family Has Glaucoma, I Would Not Get the Disease
Fact: Not all glaucoma cases are familial or hereditary, yet more than half are. Of those that are purely genetic, most occur at birth, during childhood, or young adulthood and can be recessively inherited. This means that parents may or may not have glaucoma but may carry glaucoma gene mutations that may or may not be passed on to their children.
Glaucoma can also present as a secondary condition to other health problems that increase eye pressure or block fluid drainage from the eyes. Non-genetic causes and risk factors of glaucoma include:
- Medications, such as high-dose steroids or overdosing on steroid inhalers for asthma control.
- Corrective eye surgery.
- Metabolic diseases such as diabetes, metabolic syndrome, and cardiovascular conditions.
Moreover, several risk factors can be genetic or lifestyle-related, such as hypertension or hypotension, diabetes, and other metabolic issues.
Myth: There Is Only One Type of Glaucoma
Fact: As a matter of fact, glaucoma comes in multiple varieties. The two primary forms of glaucoma[7] are angle-closure and open-angle. The most prevalent kind, known as open-angle glaucoma, is brought on by clogged drainage tubes in the eye that raise intraocular pressure over time.
On the other hand, angle-closure glaucoma is less prevalent and happens when the iris obstructs the drainage angle in the eye, abruptly raising intraocular pressure.
Other types of glaucoma include:
- Normal-tension glaucoma
- Secondary glaucoma[8] (which may be drug-induced or as a result of other eye disorders)
- Congenital glaucoma (which is present at birth)
For an accurate diagnosis and suitable management, it is crucial to speak with an eye care specialist as different types of glaucoma require different treatment approaches.
5 Glaucoma Facts Everyone Should Know
Fact: Glaucoma Is Hereditary
Four types of glaucoma are purely genetic[9]:
- Congenital glaucoma (gene mutations in CYP1B1 and LTBP2)
- Developmental glaucoma (PITX2, FOXC1, PAX6, and LMX1B)
- Juvenile primary open angle glaucoma (MYOC)
- Normal-tension glaucoma (OPTN and TBK1)
These types typically occur at very young ages in infants, children, and young adults. They may or may not be present in parents who carry these genes, and the genes may not be present or active in all children of glaucoma gene carriers.
All other cases of glaucoma have both a genetic and environmental component. It’s estimated that more than 50% of people with glaucoma have a family history of the disease and that up to 15% have a sibling with glaucoma. Having a family member with glaucoma can increase your risk by 4-10 times.[10]
If you or anyone in your family has been diagnosed with glaucoma, it is important to let the whole family know about it and to get everyone in the family to go for regular eye exams and glaucoma screening.
Fact: A Healthy Cardiovascular System Can Help Protect Against Glaucoma
While a lot of people do not worry about glaucoma if nobody has it in their family, anyone can get glaucoma if they suffer from a chronic lifestyle illness, hypertension, hypotension[11], or obesity.
Aside from medications, surgeries, and eye injuries, glaucoma risk can increase if one’s blood pressure is too high, too low[12], or if one has too many triglycerides (free fats) in their bloodstream.[13] This means that anyone with metabolic syndrome, obesity, liver disease, or a heart condition might be at risk for contracting glaucoma later in life.
For most people, these risk factors can be positively moderated through making healthy lifestyle choices, such as engaging in regular physical activity, managing stress levels, and consuming a nutritious plant-based diet.
Fact: Ethnicity Affects Glaucoma Risk
Glaucoma appears to affect African individuals more often than other ethnic groups. The African continent has shown an average glaucoma rate of 4%[14], which is much higher than any other continent around the globe, where the mean rate is usually around 2.4%. This may be related to the higher risk for hypertension seen in those with African ancestry.
Those of Inuit and Asian descent may be at a higher risk for developing rarer types of primary glaucoma, such as angle closure glaucoma. Normal tension glaucoma has the highest prevalence amongst Japanese individuals.[15]
Among elderly individuals, those of Hispanic descent over the age of 60 were at a higher risk for developing glaucoma than European counterparts.
Fact: Mid-Life Hormone Replacement Therapy May Protect Women From Glaucoma
Angle-closure glaucoma has a higher prevalence amongst aged women who are menopausal or post-menopausal[16]. Several studies over the last couple of decades have shown that hormone replacement therapy can help lower intraocular pressure as well as the occurrence of glaucoma in post-menopausal women. Scientists theorize that estrogen has a neuroprotective benefit, which can help to spare the ocular nerve. It is also a natural vasodilator.[17]
However, too much estrogen may increase the risk, and the timing of hormone replacement may as well. Some studies suggest that using the pill for longer than 5 years can increase a younger female’s risk of developing glaucoma by as much as 25% by the time she reaches her 40s.
It is unclear why the pill exerts this effect. Most contraceptive pills contain estrogen, although some may contain too much estrogen (which can cause hypotension), while others may contain too much synthetic progesterone (which can inhibit body estrogen and lead to hypertension).
Fact: Early Detection and Treatment Are Essential for Preventing Vision Loss From Glaucoma.
Early treatment of glaucoma can slow down damage to the optic nerve and prevent complete vision loss from taking over the eyes. It also allows the patient make appropriate dietary and lifestyle changes that can help to keep their blood pressure stable, improve their cardiovascular health and lose weight, as well as look after their eyes.
More than half of people with glaucoma do not know they have glaucoma[18] due to the lack of early warning signs. If someone in your family has recently been diagnosed, or if you suddenly come down with vision loss, you need to see an ophthalmologist immediately to make sure you don’t have glaucoma as well.
Conclusion
It can be a good idea for people aged 40 and over to go for regular eye exams and routine glaucoma screening to make sure they do not have the condition. If you are suffering from visual problems, you may want to get screening from an earlier age to be sure.
To search for the best Ophthalmologists, please use the Mya Care search engine.
Sources:
- [1] https://glaucoma.org/glaucoma-can-strike-at-all-ages-even-newborn-babies/
- [2] https://pubmed.ncbi.nlm.nih.gov/28505344/
- [3] https://glaucoma.org/learn-about-glaucoma/treating-glaucoma/
- [4] https://www.aoa.org/healthy-eyes/eye-and-vision-conditions/computer-vision-syndrome?sso=y
- [5] https://www.sciencedirect.com/topics/medicine-and-dentistry/trabeculectomy
- [6] https://my.clevelandclinic.org/health/diagnostics/22859-tonometry
- [7] https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/glaucoma/types-glaucoma
- [8] https://www.aao.org/education/disease-review/secondary-glaucoma-glaucoma-associated-with-acquir
- [9] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4292091/
- [10] https://glaucoma.org/glaucoma-risk-increases-in-families-spread-the-word/
- [11] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5712958/
- [12] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7141380/
- [13] https://directorsblog.nih.gov/2023/11/14/metabolomics-a-new-approach-to-understanding-glaucoma/
- [14] https://www.nature.com/articles/s41598-021-92971-w
- [15] https://glaucoma.org/are-you-at-risk-for-glaucoma/
- [16] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4326058/
- [17] https://www.aao.org/eyenet/article/glaucoma-in-women-estrogen-connection-2
- [18] https://www.cdc.gov/visionhealth/resources/features/glaucoma-awareness.html
Disclaimer: Please note that Mya Care does not provide medical advice, diagnosis, or treatment. The information provided is not intended to replace the care or advice of a qualified health care professional. The views expressed are personal views of the author and do not necessarily reflect the opinion of Mya Care. Always consult your doctor for all diagnoses, treatments, and cures for any diseases or conditions, as well as before changing your health care regimen. Do not reproduce, copy, reformat, publish, distribute, upload, post, transmit, transfer in any manner or sell any of the materials in this blog without prior written permission from myacare.com.