GLIOMA SURGERY: WHEN AND HOW IT IS DONE, RECOVERY, AND MORE
Gliomas are the most common type of malignant tumor originating in the brain, accounting for approximately 33% of all cases. Research indicates an annual incidence of approximately 6 per 100,000 individuals worldwide, with men 1.6 times more likely to be diagnosed with gliomas than women. Although a serious diagnosis, early treatment and surgery can improve the outcomes.
Surgical removal of glioma is the first choice of treatment in most cases of glioma. It’s usually followed by a comprehensive treatment plan that includes radiotherapy, chemotherapy, and post-op rehabilitation.
Brain surgery is complicated and very technically challenging. However, in recent years, Neurosurgery has come a long way. Top brain surgery centers in Germany and Europe offer the newest and most advanced surgical options for gliomas and other brain tumors, including state-of-the-art surgical technologies such as endoscopic surgery, stereotactic surgery, microscopic surgery, intraoperative neuroimaging, and intraoperative neuromonitoring (IONM). These advances have significantly improved the chances of a better quality of life and long-term survival.
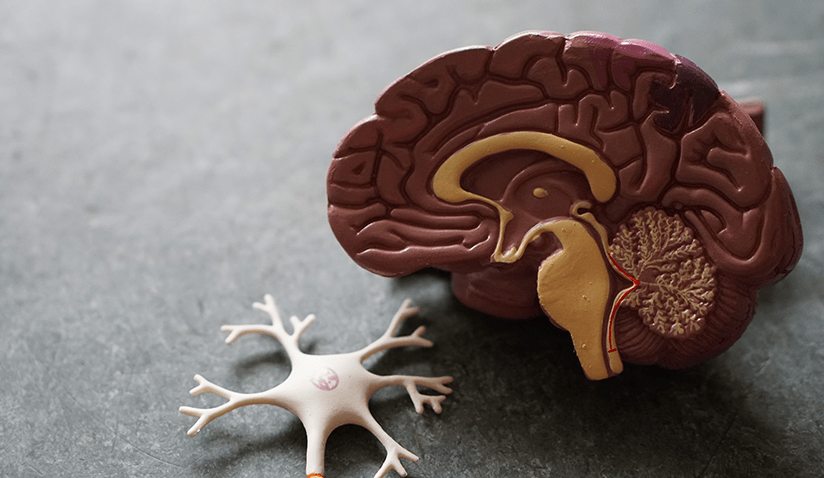
What Is a Glioma?
Gliomas are the most common primary malignant brain tumor worldwide. It usually occurs in older adults, however, it can develop at any age, including during childhood.
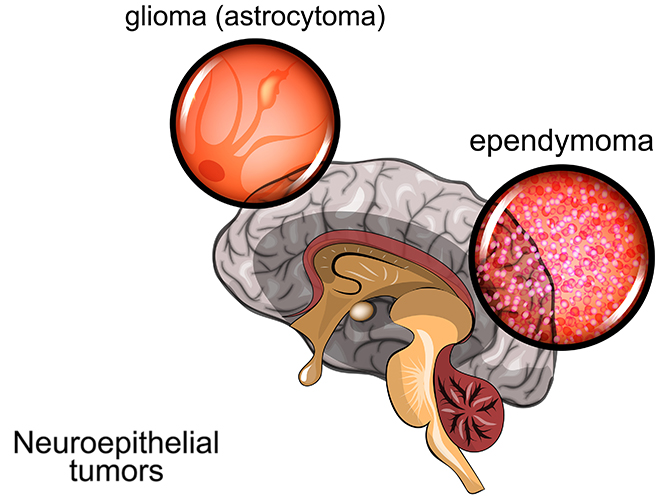
Gliomas originate from supportive cells of the nervous systems - called “glial cells”. There are several types of glial cells and, therefore, several kinds of glioma. The type of glioma tumor plays the biggest role in how quickly the cancer would advance. In general, gliomas are classified as follows:
- Astrocytoma - originating from “astrocytes” (the most common type of malignant brain cancer)
- Ependymoma - originating from ependymocytes
- Oligodendrogliomas - originating from oligodendrocytes
The classification doesn’t stop here, however. Each type of these three is further classified based on the shape and behavior of the tumor. Glioblastoma is, for example, an aggressive and rapid-growing type of astrocytoma.
Treatment of Glioma
Treating glioma can be challenging, especially if it’s an advanced and aggressive subtype. The treatment plan is multidisciplinary, with doctors and specialists from various departments taking part. Glioma treatment plan usually includes:
- Brain surgery: surgical removal of glioma, when possible, is the first choice of treatment.
- Drug therapy: Chemotherapy, immunotherapy, and targeted therapy can be administered before or after glioma surgery.
- Radiotherapy: Radiotherapy is often performed after glioma resection to kill any remaining microscopic cancerous cells. Specialized centers offer stereotactic radiotherapy; an advanced technique that helps accurately target cancerous cells without damaging any important brain functions.
When Is Glioma Surgery Needed?
Glioma surgery is usually indicated whenever it is possible. Several factors determine whether a glioma or glioblastoma can be surgically removed or not.
The location and size of the tumor usually play the biggest role in determining glioma resectability.
If it is safely possible, surgeons attempt to remove the whole tumor. If the tumor is, however, located near important nervous pathways (e.g. a pathway responsible for vision), then safe surgical removal might be challenging. In such cases, even if the whole glioma cannot be removed, partial resection can still relieve the pressure on the surrounding normal tissue and improve the quality of life of the patient.
Moreover, the experience of your neurosurgeon and the technologies available at the neurosurgery center where you’re being treated play an extremely critical role.
At top centers, brain navigation technologies (intraoperative neuroimaging and neuromonitoring) combined with microscopic glioma surgery enable safe performance of highly-challenging glioma removal surgeries.
Glioma Surgery
Glioma surgery involves several techniques and technologies:
Craniotomy
Brain surgery (craniotomy) is the standard treatment for operable glioma. There are many techniques and surgical approaches that your surgeon might choose from depending on the location, size, and type of your glioma.
Extensive preoperative diagnostic and imaging tests allow surgeons to carefully plan the best way to reach the tumor. They know exactly where and how they need to cut before the surgery even starts with the help of advanced imaging tools like 3D Brain Magnetic Resonance Imaging (MRI).
During glioma surgery, your surgeon will attempt to remove all of the visible tumor. Even if full resection is not possible, your surgeon will debulk the tumor to relieve any pressure on the surrounding normal tissue. Using a surgical microscope, surgeons can remove even the smallest extensions of the cancer that are not visible to the naked eye.
Equipped with state-of-the-art technologies that allow surgical navigation - akin to a comprehensive GPS system - surgeons can safely resect while avoiding injuring any vital nervous pathways (see below).
Endoscopic Skull Surgery
Endoscopic brain surgery is a fairly new surgical approach that’s quickly gaining popularity in the treatment of brain cancer. It’s considered minimally invasive brain surgery. Endoscopic glioma removal involves the use of an endoscope - a rod-like device with a camera and light source on its tip, connected to a screen.
The skull endoscope is advanced through the nose and into the skull to extract gliomas located in the frontal part of the brain. Endoscopic surgical tools are advanced through the endoscope to cut the tumor or burn cancerous tissue with the help of the camera feed.
Endoscopic glioma surgery requires immense skill and experience to successfully remove the tumor.
Intraoperative Imaging and Surgical Navigation
At specialized brain surgery centers, glioma surgery is guided using cutting-edge surgical intraoperative imaging techniques. This allows neurosurgeons to guide their interventions in real time as they remove the tumor.
With the help of intraoperative cerebral MRI and brain ultrasonography, your surgeon will be able to better assess the extension of the tumor and visualize any important nervous structure and vessels they need to avoid.
Intraoperative Neuromonitoring
Intraoperative neuromonitoring (IONM) is one of the latest technologies currently applied in neurosurgery. By measuring the electrical activity in different areas of the brain, the surgical team can identify important nerve tracts (e.g. those involved in hearing or vision).
Intraoperative neuromonitoring helps your surgeon navigate around them and remove the tumor more precisely without damaging any nerve tracts involved in sensation or movement.
With the support of specialized neurophysiologists in the operation theater, different types of intraoperative neuromonitoring might be performed depending on the location of the tumor. These include:
- Somatosensory Evoked Potentials (SSEP): Identifies areas responsible for deep and superficial sensation.
- Acoustically Evoked Potentials (AEP) / Auditory Evoked Potentials (AEP): Identifies nervous pathways related to hearing
- Visual Evoked Potentials (VEP): Identifies nervous pathways related to vision
- Electromyography (EMG): Identifies the important cranial nerves
- Electroencephalogram (EEG): Assesses the spontaneous electrical activity of the brain cells
- Direct Cortical Stimulation (DCS): Identifies nervous pathways responsible for controlling movement.
- Direct Nerve Stimulation (DNA)
Recovery After Glioma Surgery
Recovery after glioma surgery is different for each person. Some patients might be able to resume their normal life routines after a few weeks of surgery. However, in some patients, a more extensive rehabilitation plan might be needed.
Successful recovery after glioma removal surgery requires an extensive recovery plan and multidisciplinary cooperation. It might include:
- Physical therapy
- Occupational therapy
- Speech therapy
- Pain management
- Counseling for patients and caregivers
Aftercare teams strive to achieve the best quality of life for patients after glioma surgery.
Prof. Dr. med. Martin Scholz is the Head of the Department for Neurosurgery and Neurosurgical Intensive Care Medicine at Sana Hospitals Duisburg, one of the largest neurosurgical departments in Germany with expertise in all areas of microsurgery and neuroendoscopy. Professor Scholz has a special research interest in intraoperative brain ultrasonography for glioma removal. He has published several studies that highlight the important role of this advanced tool in improving outcomes and allowing for more accurate and safer resection. Supported by cutting-edge medical technologies and more than 35 years of experience, Prof. Dr. Scholz and his team routinely perform challenging glioma procedures with excellent outcomes.
Sources:
- Endoscopy in Temporal Lobe Glioma and Metastasis Resection: Is There a Role?
- Intraoperative Neurophysiological Monitoring
- The value of intraoperative ultrasonography during the resection of relapsed irradiated malignant gliomas in the brain
- The value of intraoperative sonography in low grade glioma surgery | Request PDF
- John Hopkins Medicine - Health Conditions - Gliomas
Disclaimer: Please note that Mya Care does not provide medical advice, diagnosis, or treatment. The information provided is not intended to replace the care or advice of a qualified health care professional. The views expressed are personal views of the author and do not necessarily reflect the opinion of Mya Care. Always consult your doctor for all diagnoses, treatments, and cures for any diseases or conditions, as well as before changing your health care regimen. Do not reproduce, copy, reformat, publish, distribute, upload, post, transmit, transfer in any manner or sell any of the materials in this blog without prior written permission from myacare.com.