THYROID SURGERY (INCLUDING MINIMALLY INVASIVE APPROACHES)
Thyroid diseases are extremely common and can occur at any age. In about one in three adults in Germany, at least one pathological thyroid alteration develops in the course of a lifetime.
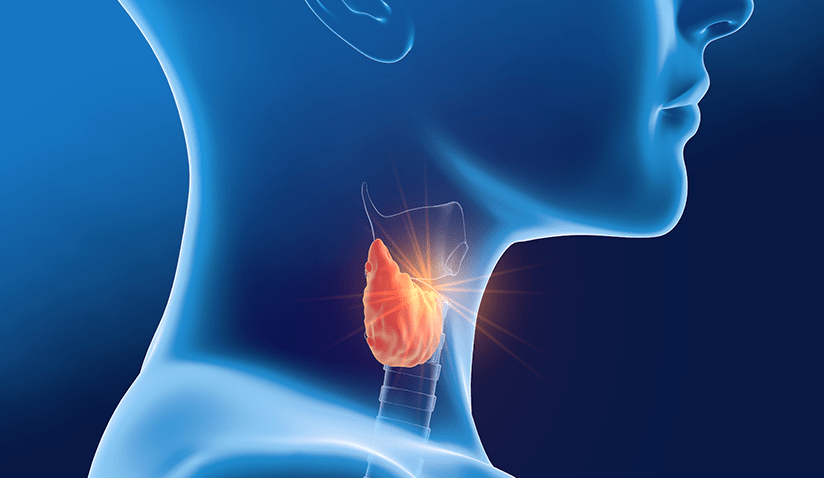
In general, a distinction is made between hormonal dysfunctions (e.g. hyperthyroidism and hypothyroidism) and changes in size and condition (enlargements, nodules, tumors) of the thyroid gland.
Often there are combinations and mixed forms. However, a structural alteration does not necessarily reflect the function of the organ, and vice versa. In other words, patients with a normal-sized and nodule-free thyroid gland can suffer from hyperthyroidism. On the other hand, patients with very large thyroid nodules or even with malignant tissue neoplasms (cancer) can also have completely normal thyroid levels in their blood.
When Is Thyroid Surgery Necessary?
Various therapeutic procedures are available for the treatment of thyroid disorders. The necessity of a surgery for thyroid varies and good medical consultation requires a diagnosis that is as exact as possible. Whether and how emergent thyroid surgery is depends on the specific kind of thyroid disease, the individual findings and, of course, the patient's preferences.
A clear surgical requirement exists for malignant diseases and diseases suspected of being cancerous, e.g.
- thyroid cancer
- thyroid nodules indicative of cancer
Thyroid surgery may also be necessary for benign conditions, e.g.:
- symptomatic thyroid enlargement (struma)
- glandular proliferation (adenoma)
- cavity formation (cyst)
- hyperthyroidism
- Basedow's disease
- Thyroiditis
In general, surgery is always recommended if an enlargement or nodule formation causes subjective discomfort or unpleasant sensations, e.g.
- compulsion to clear the throat
- lump, tightness, pressure or foreign body sensation in the throat
- swallowing difficulties
- breathing difficulties
- hoarseness
This also applies to objectifiable conditions such as:
- constriction or displacement of the trachea
- constriction or displacement of the esophagus
- hoarseness due to pressure damage of the vocal cord nerve
- extension of the thyroid gland into the thorax
Often several reasons exist for thyroid surgery and in each case the arguments for or against surgery may vary. In addition, possible treatment alternatives must be discussed as well.
Types of Thyroid Surgery
Thyroid Resection Procedures
Depending on where and how much thyroid tissue is removed, a distinction is made between different types of surgery (resections).
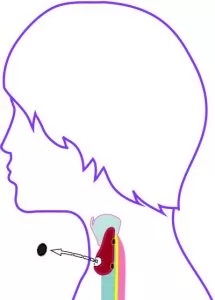
In limited operations, the pathological finding is removed from the thyroid gland either along its capsule (enucleation) or with a fringe of healthy thyroid tissue (wedge excision). If the pathological alteration is limited only to the tissue bridge between the two lobes of the thyroid gland (isthmus), only this tissue bridge may be removed (isthmus resection).
 |
 |
 |
These limited procedures are only used when there is an isolated pathological finding in an otherwise healthy thyroid gland. This usually exists only in the case of smaller nodules or cysts, however, it can be usually decided only during surgery whether a limited resection is appropriate.
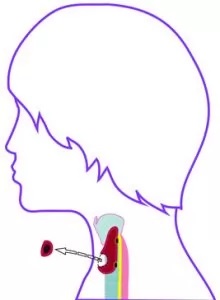
Depending on how much tissue can be left, these types of thyroid surgeries are called subtotal flap resection (thyroid remnant about 4 grams and less on one side), near-total flap resection (thyroid remnant 1 gram and less on one side) or complete flap resection (hemithyroidectomy, no remnant on the operated side). Depending on the extent of the disease, these procedures can be performed on only one side of either thyroid lobe or in all possible combinations on both thyroid lobes simultaneously. Complete removal of the thyroid gland is called total thyroidectomy.
 |
 |
 |
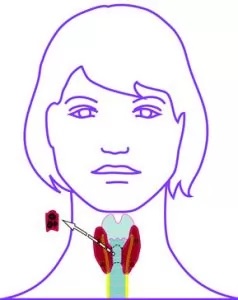
Minimally Invasive Approaches
In conventional surgery, the skin incision is made on the front of the throat in the lower parts (Kocher`s collar incision). With a well-planned incision and an aesthetic suture technique, very pleasing results can usually be achieved. In order to keep the scars as small and invisible as possible, various minimally invasive surgical techniques have been developed in recent years.
...with incision on the throat:
To improve the aesthetic result, the skin incisions on the throat are made as short and concise as possible. Special instruments are used to visualize and operate on the thyroid gland either under direct vision (e.g. MIT, Minimally Incisional Thyroidectomy) or via a miniature camera (MIVAT, Minimally Invasive Video Assisted Thyroidectomy).
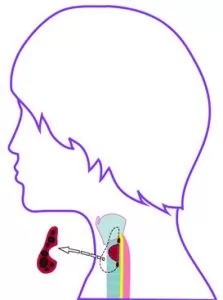
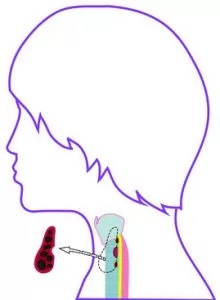
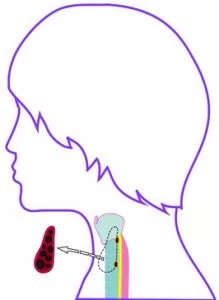
...without incision on the throat:
In other minimally invasive approaches, the incisions are not located in the visible throat areas. In the ABBA method (axillo-bilateral-breast approach), for example, two incisions are made at the edge of the right and left nipple and in the right or left armpit. The surgical instruments and camera are guided under the skin to the thyroid gland. Since the surgical specimen must be removed through one of these approaches, this method is suitable only for a few and very small thyroid alterations.
Microsurgical techniques
One key objective of modern thyroid surgery is the greatest possible protection of vulnerable structures, such as the fine vocal cord nerves or the small parathyroid glands. These structures can be optically magnified by means of aids and thus better recognized and protected.
If very precise surgical instruments are used, relevant procedures can be performed using microsurgical techniques. This is helpful when, for example, a vocal cord nerve needs to be gently dislodged from surrounding adhesions and nodules or tumors.
Intraoperative neuromonitoring
Intraoperative neuromonitoring facilitates the protection of nerves. This is based on the principle of "stimulation and stimulus response". Using a fine probe, the surgeon can regularly send minimal electric shocks during the operation. If the irritated structure is the vocal cord nerve and it is intact, the nerve transmits the impulse to the responsible laryngeal muscle and the vocal cord opens.
This is usually controlled by means of a special ventilation tube. The tube is a silicone tube that is inserted between the patient's vocal cords into the trachea during every general anesthesia to ventilate the patient. For neuromonitoring, fine electrodes are incorporated at the level of the vocal cords.
Protection of the parathyroid glands
Special attention is also paid to the small parathyroid glands. Sometimes they have no independent blood supply, but are supplied by blood vessels of the thyroid gland. In this case, the parathyroid glands may suffer from reduced blood supply after the organ has been removed. Intraoperative parathyroid hormone determination can be used to detect or rule out a drop in hormone levels during surgery.
The functionality of a poorly perfused parathyroid gland can be preserved by auto-replantation. A parathyroid gland of this type is first removed, cut into many pieces of tissue, and replanted into a muscle pocket in the surgical area with a good blood supply.
Risks and complications of thyroid surgery
With an experienced surgeon, the removal of the thyroid gland usually proceeds without complications. The general surgical risk of pneumonia, thrombosis, heart attacks, etc. is minimal and the surgical mortality rate after thyroid surgery is close to zero.
So-called procedure-specific complications of thyroid surgery consist mainly of problems with wound healing, post-operative bleeding, hematoma formation, and damage to the vocal cord nerves or disturbances in calcium metabolism.
- Inflammation and wound healing problems: Despite all precautions, inflammation and impaired wound healing can occur with any surgery. With consistent and proper treatment, infections and wound healing problems usually resolve after thyroid surgery.
- Bleeding, hematoma: After thyroid surgery, more severe bleeding, post-operative bleeding or major hematoma are very rare. Reoperation may be needed to stop secondary bleeding or remove any bruising. Such revision surgeries are usually performed within the first 24 hours after the initial surgery and heal without any further repercussions.
- Voice and speech disorders: Due to the close anatomical proximity of the thyroid gland to structures involved in voice generation, thyroid surgery may result in changes in the voice. Damage to the vocal cord nerves can result in paralysis of the vocal cord (recurrent paresis). However, in the course of time, they completely resolve themselves. Due to modern surgical techniques and the use of technical aids, the risk of permanent damage to the vocal cord nerves (permanent recurrent paresis) is low with an experienced thyroid surgeon and is at or even below 1% in very good hospitals.
Patients with vocal cord paralysis are not speechless, they can talk and communicate, but their voice usually sounds hoarse, soft or croaky. Most postoperative recurrent paresis results from strain or traction on the vocal cord nerve and improves on its own as it progresses. Satisfactory vocal function can often be achieved with speech therapy, even in cases of permanent vocal cord paralysis. If this is not successful, endoscopic corrective measures on the vocal cords are also available. - Hypofunction of the thyroid (hypoparathyroidism): During thyroid surgery, the parathyroid glands located directly behind the thyroid gland may also be damaged or even inadvertently removed. In this case, there may be a postoperative drop in calcium in the blood. In excellent hospitals, the risk of permanent hypoparathyroidism is at or even below 1%.
Benefits of Thyroid Surgery
For the treatment of thyroid disease, surgery on the thyroid gland offers some very significant advantages compared to other therapies:
- Immediate onset of effect: Surgery is the only treatment where the desired effect (e.g. size reduction, elimination of hormone overproduction) occurs immediately after the surgery. In case of a successful course of treatment, surgery with outpatient suture removal is completed after only a few days.
- Individual and condition-specific therapy: During thyroid surgery, all pathological alterations (for example, warm and cold nodules, inflammations) can be treated simultaneously and immediately. There is also the possibility of individual and condition-specific treatment, ranging from sparing partial removal to complete removal of the entire thyroid gland.
- Definitive diagnosis: Currently, a definitive, i.e. a 100% distinction between benign and malignant, is only possible by pathological examination of surgically removed thyroid tissue. This is a very decisive advantage for all findings indicative of tumor.
Prof. Dr. med. Hans Udo Zieren is head of the department for thyroid and parathyroid at Sana Hospital Hürth (Cologne) and has more than 30 years of experience in thyroid surgery. Together with his surgical team, he has already performed more than 10,000 thyroid and parathyroid surgeries for patients from all over Germany and abroad. His treatment spectrum ranges from surgeries of all degrees of difficulty, often highly complex cancer and recurrent operations. In addition to all types of conventional surgical procedures for benign and malignant diseases, Professor Zieren also performs minimally invasive treatment methods such as nodule destruction by thermoablation. Prof. Dr. Hans Udo Zieren is also the founder and medical director of the German Thyroid Center - a platform of physicians from various specialties who are focusing on the thyroid gland from different perspectives.
Sources:
- https://www.deutsches-schilddruesenzentrum.de/wissenswertes/schilddruesenerkrankungen/
- https://www.deutsches-schilddruesenzentrum.de/wissenswertes/behandlung/schilddruesenoperation/
Disclaimer: Please note that Mya Care does not provide medical advice, diagnosis, or treatment. The information provided is not intended to replace the care or advice of a qualified health care professional. The views expressed are personal views of the author and do not necessarily reflect the opinion of Mya Care. Always consult your doctor for all diagnoses, treatments, and cures for any diseases or conditions, as well as before changing your health care regimen. Do not reproduce, copy, reformat, publish, distribute, upload, post, transmit, transfer in any manner or sell any of the materials in this blog without prior written permission from myacare.com.