ANDROPAUSE AND MALE AGING: SYMPTOMS, TREATMENT OPTIONS AND LIFESTYLE SUGGESTIONS
Andropause is another way of saying “male menopause” and tends to refer to the hormonal decline seen in male aging. Doctors are still debating whether men actually go through a male version of menopause or whether andropause is a form of hypogonadism that affects a large percentage of the aged male population.
Unlike in women, sex hormones in men do not just stop when aging hits but see a progressive decline. In healthy men, this decline is so gradual that it may only affect a man in his 80s or later. In men who are predisposed to hypogonadism, low testosterone levels may affect reproductive function as early as age 45-50 with symptoms becoming full-blown at later ages (70+) on average.[1]
What Causes Andropause?
The main cause of “andropause” is low testosterone levels. Testosterone is seen to decline approximately 1% a year from the time a man is between 30 and 40 years of age[2], being roughly 65% the levels seen in youth on average when a man reaches his 70s.[3]
Testosterone is made by Leydig cells in the testes. The testes are instructed to produce testosterone by the hypothalamus and pituitary gland which release gonadotropin-releasing hormone and gonadotropins such as luteinizing hormone respectively. Luteinizing hormone stimulates an increase in testosterone production and is released from the brain in a series of pulses at different times of the circadian cycle.
Its production is a virtually stable process that can theoretically last a man his entire life and longer. Modern living and age-related factors however can catch up with a man and decrease testosterone production. These include increased frequency of contracting infections, nutritional deficiencies, heightened emotional stress and reduced physical activity.
Certain metabolic diseases such as diabetes and obesity can increase the risk for hypogonadism[4] and a percentage of young men with these conditions already suffer similar symptoms from low testosterone levels. Damage to the testes can also result in lower testosterone production, as can a higher intake of pollutants such as cadmium.
Intriguing studies highlight that in populations of tribal men, andropause is far rarer than in the West and testosterone levels of tribal men remain more constant than seen in Western counterparts. [5]
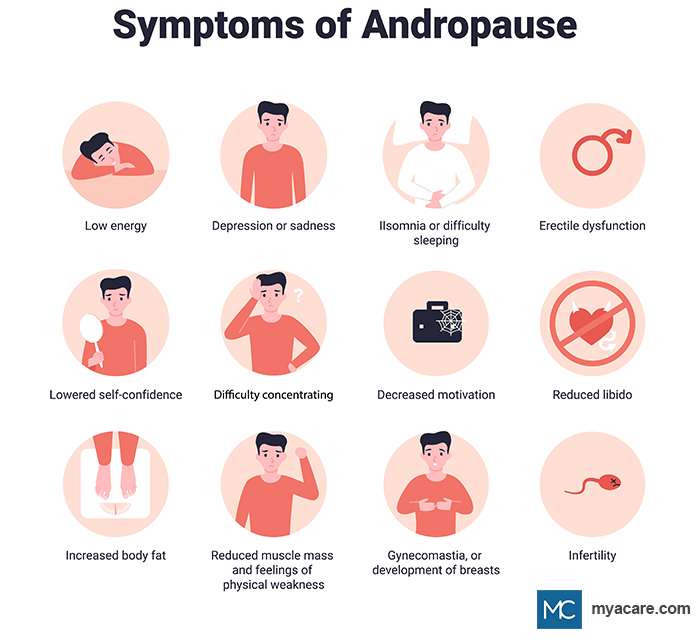
Andropause Symptoms
Symptoms of andropause are the same as hypogonadism, testosterone deficiency and the late stages of male aging[6]. They include:
- Prostatic enlargement
- Loss of libido
- Reduced sexual function
- Lower energy levels
- Muscle weakness
- Depression
- Reduced immune function
Some men also get hot flushes similar to women with menopause. Sleep disturbances, mood swings (especially irritability) and abdominal weight gain are other symptoms associated with male aging[7]. Eventually testosterone deficiency can result in issues with urination and erectile dysfunction.
Complete cessation of testosterone production still does not occur in male menopause, but does occur in the cases of prostatic cancer and either chemical or physical castration.
Diagnosing Andropause
Andropause is not an official condition that can be diagnosed, however low testosterone levels and hypogonadism can be diagnosed. As can a condition that is associated, such as benign prostatic hyperplasia. The majority of men ignore symptoms that crop up with moderate testosterone decline and therefore a diagnosis of hypogonadism tends to only be achievable when symptoms start to impact on the quality of life.
A doctor will first take a case history and if symptoms add up, they will first likely check the prostate to make sure it’s not prostate enlargement that is causing the problem. After a physical examination, blood tests may be ordered to test hormone levels as well as markers for other reproductive abnormalities. In the absence of disease, testosterone decline or deficiency can then be diagnosed. Full blown deficiency tends to affect less than 20% of men in their 70s and even less in younger aging men.[8]
As testosterone levels fluctuate throughout the day, it should be noted that blood tests may need to be repeated in order to improve the accuracy of the results.
Benign Prostatic Hyperplasia: A Common Theme in Male Aging
Benign prostatic hyperplasia (BPH) is a far more likely diagnosis for an elderly man with persistent urinary and reproductive symptoms. This condition occurs in up to 90% of all aged men living a modern lifestyle after reaching their 80s or 90s and is caused by disruptions in prostatic androgen signaling[9] [10].
The disease is a product of high prostatic testosterone, particularly its more potent form, dihydrotestosterone (DHT). DHT has a potency of up to 10 times that of normal testosterone and causes the gland to grow much larger. [11]
Eventually the gland can partially block the urinary tract, creating irritation, pain and other problems while passing urine. Over time, the bladder and nervous system also become impacted, creating bladder obstructions, false sensations of urinary urgency and sleep disruptions.
The levels of testosterone in the bloodstream do not necessarily reflect the levels in the prostate. Even though hormones decline with aging, prostatic testosterone levels increase in the case of BPH, making testosterone replacement therapy a dangerous option to these men. In spite of the danger, some men with BPH show improvements in their urinary symptoms in response to testosterone treatment. This is hypothesized to be a result of metabolic improvement.[12]
Andropause Treatment Options
While there is no cure for old-age; men with declining testosterone levels have a few options available to help ease symptoms associated with “andropause.”
1. Lifestyle Considerations
Before any treatments are prescribed for aging men, lifestyle considerations and appropriate changes should be made. It is common knowledge that aging and disease are both heavily influenced by poor nutrition, living a sedentary lifestyle, excessive alcohol consumption and smoking.[13] [14] Testosterone production is also known to be influenced by nutrition and metabolism, as evidenced by hypogonadism in obese men and men with metabolic syndrome.[15] Men who consumed lots of processed bread, pastries, dairy, desserts, and take-out meals and who consumed little dark green vegetables and home-cooked foods tended to have low testosterone levels.
In this respect, increasing nutrition, keeping active, limiting both alcohol consumption and smoking can improve parameters of aging. As one ages, digestion tends to become problematic, resulting in nutrient malabsorption and age-related deficiency. Furthermore, aged individuals tend to eat less and feel less hungry on average, further diminishing nutritional intake, physical capacity and physical activity.[16]
Increasing dietary intake of water-soluble fiber, dark green leafy vegetables, water, and foods rich in digestive enzymes (such as fruit and probiotics) can help increase nutrient absorption. Multi-mineral and multi-vitamin supplements may also be indicated[17]. However, in the absence of disease, studies suggest that the effects of supplementation are minimal compared to consuming a healthy variety of wholefoods (fruits, vegetables, nuts, seeds, grains, etc).
2. Androgen Replacement Therapy
Generally, androgen supplementation is only prescribed on a short term basis to those who are deficient due to full-blown hypogonadism in the absence of disease.
In this respect, hormone replacement therapy is becoming an increasingly popular option for aging men[18]. Some men receive benefit from supplementing on androgens, including an increased libido, less fatigue and improved mood[19]. Animal studies revealed that testosterone therapy may help improve reduced bone density associated with andropause.
However, studies convey contradicting results about testosterone replacement therapy for aged men. The most benefit appears to be received when care is taken to ensure that hormone levels remain within healthy parameters. Increasing testosterone levels may cause an increase in the production of testosterone-derived hormones, including DHT and estradiol, both of which can exacerbate the onset of BPH.
Side Effects
Adverse effects associated with androgen replacement therapy include increased red blood cell production and decreased HDL cholesterol production. In transdermal applications, testosterone therapy induced flushing, acne, and oily skin.[20]
Research is limited on the long term effects of androgen supplementation.
Contraindications
Testosterone supplements are contraindicated for men with prostate cancer, benign prostatic hyperplasia and lower urinary symptoms or LUTS. Those with obstructive sleep apnea, kidney disease and cardiovascular disease should also avoid testosterone supplementation.
3. Medication
In men with prostatic enlargement as a result of aging, medications that manage symptoms are generally the first line of treatment[21].
The doctor might prescribe the following types of drug:
- Alpha Blockers which block conduction of nerves to the prostate and help to lower prostatic contractions that result in urinary blockages.
- 5-Alpha-Reductase Inhibitors that prevent the conversion of testosterone into DHT. This may help to lower the size of the gland and slow its growth.
- PDE-5 Inhibitors can help lessen erectile dysfunction, which is a common side effect of using alpha blockers and/or of testosterone deficiency.
Side Effects
Alpha blockers can cause dizziness, headaches, increased heart rate and weakness, especially when taken on the first dose. [22]
5-alpha-reductase inhibitors may contribute towards hair loss, hypogonadism, depression, decreased fertility[23] and erectile dysfunction.
PDE5 inhibitors might induce headaches, gastric reflux, flushing, muscle stiffness, back pain, low blood pressure, weakness, and dizziness. Severe side effects include irreversible vision and hearing loss. [24]
Contraindications
Alpha blockers are contraindicated in the case of kidney impairment, history of cataract surgery, cerebrovascular disease, coronary artery disease and active respiratory infection.[25]
5-alpha-reductase inhibitors are contraindicated for men with hypogonadism who do not have prostatic enlargement.
PDE5 inhibitors should not be taken by those who are at an increased risk for acquiring prostate and skin cancer as it may exacerbate disease onset.
Any medication is contraindicated in the case of being allergic to any of the ingredients.
4. Prostate Surgery
Surgical options for prostatic enlargement are only employed when symptoms get out of hand and threaten to cause bladder obstruction. Your doctor will only prescribe surgery when medication is non-responsive or symptoms require drastic action to be taken. [26]
The most common surgical procedure pertaining to the aging prostate would be a transurethral prostatic resection. The surgeon inserts a surgical tool through the urethra known as a resectoscope (similar to a larascope). This tool allows for the physician to see the enlargement and to cut away overgrown prostatic tissue that is causing a urinary blockage.
As this does not address the underlying cause of the issue, transurethral resections may need to be repeated after some time when the prostate grows back.
Some men opt for a prostatectomy in which the whole gland is removed. A doctor may suggest prostate removal if the gland is 100g or more (a normal size is roughly 22g on average).
Side Effects
Both types of surgery (especially full prostate removal) may cause “dry ejaculation” in which the ejaculate moves the wrong way and does not exit at the time of orgasm. This can result in male infertility, yet does not usually interfere with any other aspect of reproduction.
Urinary tract infections are common complications after prostate surgery, as is painful urination for a few days post-surgery.
Rare complications of transurethral resection include[27]:
- Erectile dysfunction
- Loss of bladder control
- Heavy bleeding
- Transurethral resection syndrome in which blood potassium drops dangerously low
Contraindications
Blood thinning medications and over-the-counter painkillers ought to be avoided a few days before surgery as they count as contraindications.
Those with high blood pressure or kidney disease should not opt for prostate surgery due to the risk (even while low) of transurethral resection syndrome.
5. Botox Injections
Botox is a risky (unofficial) treatment option that has been shown to be effective in some but not all cases of BPH, LUTS or overactive bladder[28]. It’s mainly used as an alternative to medical treatment for unresponsive cases where severe urinary symptoms are concerned and where the patient is not a good candidate for surgery.
The theory behind it is that botox injected into the prostate can relax the muscles in the gland by blocking nerve conduction to it. Botox contains botulin toxin A which is a highly toxic substance that paralyzes nerves when injected into them[29]. The body takes a long time to remove botox, sealing it off at the injection site from the rest of the body and degrading it over the course of 2 years or longer. In some with chronic diseases that affect immune function, botox has been shown to create a systemic infection, adding to the treatment risk.
Previous studies have shown that it has the same efficacy as a placebo treatment, depending on the site of injection, who administers the treatment and the unique disposition of the patient.
A French study managed to improve the quality of life for 58% (37 out of 62) of men with BPH who received prostatic botox injections[30]. These results lasted for up to 18 months. Other studies reveal very low reductions in prostate size, improvements in urination and other benefits lasting for up to 3[31] and 6 months[32].
Side effects
No side effects have been observed for prostatic botox injections, as of yet. A lot more research and long-term follow up studies need to be conducted before one can rule out the possibility for potential adverse reactions to botox.[33]
Contraindications
Botox is contraindicated for those with active urinary tract infections, recurring urinary tract infections or who are allergic to botulin toxin. It is also contraindicated for those with motor neuropathies such as parkinson’s disease or when using prescription muscle relaxants.
6. High-Intensity Focused Ultrasound Technology
Ultrasound technology has been silently available as an option for men with prostatic enlargement and urinary symptoms since the late 90s. High intensity energy from an ultrasound device can improve symptoms through thermally ablating prostatic tissue that is placing pressure on the urethra[34].
Men with BPH have been shown to benefit from ultrasound treatment in this manner, with result remaining stable over a year after treatment.[35] A longer term study revealed that the treatment results are not indefinite and that more than 40% of men in the study opted for surgery within 1 month to 4 years of ultrasound treatment.[36]
Side Effects
Side effects are similar to those of surgical transurethral resection of the prostate, with the inclusion of rectal burns as a rare complication.[37]
Contraindications
Ultrasound is contraindicated in the event of urinary tract infection, bladder stones, hypertension, arteriosclerosis or in diseases where optimal blood coagulation is compromised. [38]
Conclusion
There is still debate as to whether andropause is a real condition or not. However, it is clear that blood testosterone levels tend to decline slowly in aging men, while tending to show an increase in the prostate. These age-related changes can be improved through healthy dietary and lifestyle choices and may also see improvements with testosterone treatment, in spite of inconclusive evidence.
In the event of disease such as prostatic enlargement, prescription drugs are advised. Surgery, botox and high-intensity ultrasound are other options for those with prostatic enlargement who do not respond to medications.
It is important to discuss any age-related treatment or therapy first with a healthcare professional, especially if disease is suspected, already present or if one is taking other medications that may cross-react.
To search for the best Urology healthcare providers in Croatia, Germany, India, Malaysia, Singapore, Spain, Thailand, Turkey, Ukraine, the UAE, the UK and the USA, please use the Mya Care search engine.
Sources:
- [1] https://www.webmd.com/men/guide/male-menopause
- [2] https://academic.oup.com/biomedgerontology/article/57/2/M76/547924
- [3] https://pubmed.ncbi.nlm.nih.gov/10687877/
- [4] https://pubmed.ncbi.nlm.nih.gov/29658833/
- [5] https://academic.oup.com/biomedgerontology/article/70/10/1262/2605487
- [6] https://pubmed.ncbi.nlm.nih.gov/15660505/
- [7] https://pubmed.ncbi.nlm.nih.gov/12088183/
- [8] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4440190/
- [9] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3826535/
- [10] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3350783/
- [11] https://pubmed.ncbi.nlm.nih.gov/12657354/
- [12] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4650459/
- [13] https://pubmed.ncbi.nlm.nih.gov/23522750/
- [14] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5227979/
- [15] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6266690/
- [16] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6064642/
- [17] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5984649/
- [18] https://www.mayoclinic.org/healthy-lifestyle/mens-health/in-depth/male-menopause/art-20048056
- [19] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4046605/
- [20] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4921612/
- [21] https://pubmed.ncbi.nlm.nih.gov/26676726/
- [22] https://www.mayoclinic.org/diseases-conditions/high-blood-pressure/in-depth/alpha-blockers/art-20044214
- [23] https://www.statpearls.com/ArticleLibrary/viewarticle/16992
- [24] https://www.ncbi.nlm.nih.gov/books/NBK549843/
- [25] https://www.ncbi.nlm.nih.gov/books/NBK556066/
- [26] https://www.mayoclinic.org/tests-procedures/turp/about/pac-20384880
- [27] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6202296/
- [28] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4848615/
- [29] https://www.health.harvard.edu/newsletter_article/Botox_and_the_prostate_A_new_wrinkle
- [30] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5780293/
- [31] https://pubmed.ncbi.nlm.nih.gov/31189024/
- [32] https://pubmed.ncbi.nlm.nih.gov/19057212/
- [33] https://pubmed.ncbi.nlm.nih.gov/19887944/
- [34] https://www.fusfoundation.org/diseases-and-conditions/urological/benign-prostatic-hyperplasia-bph
- [35] https://pubmed.ncbi.nlm.nih.gov/8587227/
- [36] https://pubmed.ncbi.nlm.nih.gov/10828669/
- [37] https://www.openaccessjournals.com/articles/a-technical-update-of-highintensity-focused-ultrasound-ablation-for-prostate-cancer-and-benign-prostatic-hyperplasia-12802.html
- [38] https://www.ncbi.nlm.nih.gov/books/NBK547717/
Disclaimer: Please note that Mya Care does not provide medical advice, diagnosis, or treatment. The information provided is not intended to replace the care or advice of a qualified health care professional. The views expressed are personal views of the author and do not necessarily reflect the opinion of Mya Care. Always consult your doctor for all diagnoses, treatments, and cures for any diseases or conditions, as well as before changing your health care regimen. Do not reproduce, copy, reformat, publish, distribute, upload, post, transmit, transfer in any manner or sell any of the materials in this blog without prior written permission from myacare.com.