Cyberknife: Precise, Non-Invasive, Robotic Radiation Therapy
Medically Reviewed by Dr. Aurora Rodríguez and Dr. Rafael García
About CyberKnife and How it Works
CyberKnife vs. Other Radiation Therapies
Since its inception, the primary objective of radiotherapy has been to administer the maximum dose of radiation to the tumor or lesion, thereby achieving the greatest local control while minimizing the dose to surrounding healthy tissues. This relationship, known as the index or therapeutic window, has been strengthened thanks to technological advances in recent years.
Radiotherapy has seen remarkable progress over the decades, advancing from basic 2D treatments to highly sophisticated, image-guided techniques. Key milestones include the shift to CT-based planning, the introduction of 3D conformal radiotherapy, and the rise of intensity-modulated radiotherapy (IMRT), all of which improved precision and safety. A major leap came with the advent of stereotactic approaches and radiosurgery, which enable high-dose radiation (ablative doses) to be delivered with superior accuracy in fewer sessions (usually between 1 and 5). These developments paved the way for technologies like CyberKnife, which integrate robotics, real-time imaging, and motion tracking to deliver precise, non-invasive radiation therapy across a wide range of conditions.
Types of Radiation Therapy
Understanding how radiation therapy is categorized helps clarify where Cyberknife fits in. Radiotherapy techniques are mainly defined by how radiation is delivered.
1. External Beam Radiation Therapy (EBRT): Delivers radiation from an external source. This includes:
- Conventional (2D) Radiation Therapy: Utilizes two-dimensional imaging for treatment planning.
- 3D Conformal Radiation Therapy (3D-CRT): Shapes radiation beams using 3D imaging to match the tumor.
- Intensity-Modulated Radiation Therapy (IMRT): Varies beam intensity, enabling precise dose distribution and minimizing exposure to healthy tissue.
- Image-Guided Radiation Therapy (IGRT): Utilizes image guidance during treatment, increasing precision, safety, and accuracy.
- Stereotactic Radiosurgery (SRS) and Stereotactic Body Radiation Therapy (SBRT): Highly focused treatments delivering high doses to small, well-defined brain (SRS) or body (SBRT) tumors in one or a few sessions, minimizing damage to healthy tissue.
- Particle Therapy: Uses particles like protons for highly precise targeting, minimizing damage to healthy tissue.
2. Brachytherapy (Internal Radiation): Places radioactive sources inside the body, near or inside the tumor; commonly used for prostate, cervical, and breast cancers.
3. Systemic Radioisotope Therapy: Administers radioactive substances orally or by IV to target cancer throughout the body (e.g., radioactive iodine for thyroid cancer).
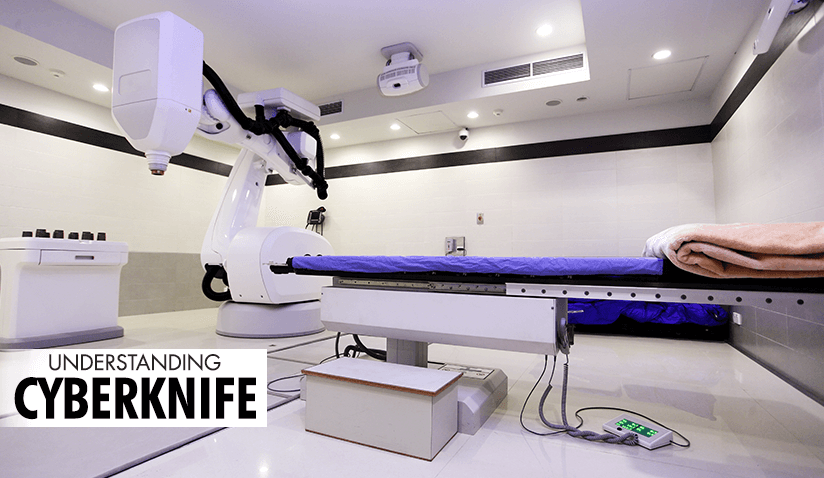
What is CyberKnife and How Does It Work?
Over 40 years ago, the first radiosurgeries were performed on the brain with Gamma Knife. However, extending the positive outcomes of brain radiosurgery to other parts of the body was not feasible until precise movement control became possible.
CyberKnife is a non-invasive robotic radiation therapy system designed to deliver precise, high-dose radiation to tumors and other abnormalities. It was initially approved as a stereotactic radiosurgery for treating brain and skull-base tumors, later expanding in scope as an advanced form of stereotactic body radiation therapy for other anatomical locations.
The technology integrates a linear accelerator mounted on a robotic arm with real-time image guidance, ensuring accuracy, optimal radiation delivery, and patient comfort without requiring invasive procedures or rigid immobilization devices. The system continuously monitors tumor position using advanced imaging, making it especially effective for treating tumors that may shift during the procedure, such as those in the lungs, liver, pancreas, kidney, or prostate.
The robotic arm moves around the patient, delivering radiation from multiple angles with sub-millimeter accuracy. The linear accelerator, which is mounted on the robotic arm, uses electricity to speed up particles (electrons) and create high-energy X-rays that are carefully shaped and aimed. This limits radiation exposure to surrounding healthy tissue, minimizing side effects while maximizing tumor control.
Comparing CyberKnife to Other Radiation Therapies
CyberKnife vs. Conventional (3D) Radiation Therapy
Traditional 3D radiation therapy uses X-rays to deliver radiation from a fixed direction, often affecting healthy tissues surrounding the tumor. CyberKnife, in contrast, offers a robotic, image-guided approach that continuously tracks tumor movement and adjusts radiation beams in real time. This results in higher precision, reducing damage to healthy tissues and minimizing side effects.
Furthermore, CyberKnife utilizes single fraction and hypofractionation, meaning it can deliver radiation in fewer sessions by using higher doses per treatment. Traditional radiation therapy often requires daily sessions for several weeks, while CyberKnife can complete treatment in one to five sessions, depending on the tumor type and location.
CyberKnife vs. Other External Beam Radiation Therapies
| Feature | CyberKnife | Tomotherapy | Gamma Knife | Proton Therapy | TrueBeam |
|---|---|---|---|---|---|
| Radiation Type | X-rays (photons) | X-rays (photons) | Gamma rays | Proton beams | X-rays (photons) or electrons |
| Delivery Method | Robotic arm with multiple angles | Helical delivery (like a CT scanner) | Fixed beams from a helmet-like device | Pencil-beam scanning | Gantry-based; Single or multiple 360-degree rotational arcs |
| Tracking/ Targeting | Real-time tumor tracking | Image-guided with CT-like scanning | Fixed stereotactic frame | Advanced imaging but less real-time tracking | Imaging with positioning adjustments |
| Invasiveness | Non-invasive | Non-invasive | Frame-based (may require head screws) | Non-invasive | Non-invasive |
| Precision | Sub-millimeter accuracy | High | High (but limited to the brain and head) | Very high | High |
| Number of Sessions & Duration | 1-5 sessions (each 15-60 min) | Multiple sessions | 1 session | Fewer sessions than traditional X-ray therapy | Variable |
| Indications & Treatment Areas |
Brain, spine, lungs, prostate, liver, pancreas, lymph nodes, head and neck, adrenal glands, and kidneys. Certain pediatric tumors. Re-irradiation. |
Brain, spine, head & neck, body tumors | Brain and head only | Brain, lung, prostate, pediatric tumors | Broad applications |
| Technology Type | Robotic image-guided LINAC | Helical LINAC | Stereotactic radiosurgery (SRS) | Particle accelerator | Linear accelerator |
| Motion Management | Tracks tumor motion in real-time | No direct motion tracking | No motion tracking (fixed frame) | Adjusts for organ motion | Imaging-guided but less real-time tracking |
| Anesthesia | Not required | Not required | May require local anesthesia for setting the head frame | Not required | Not required |
CyberKnife vs. Surgery
CyberKnife can be a non-invasive alternative to surgery for certain cancers and conditions, particularly when traditional surgery is too risky or when patients prefer a less invasive approach.
When is CyberKnife a Potential Alternative to Surgery?
- Patients who are ineligible for surgery owing to age, medical conditions, or tumor location.
- Tumors near critical structures, where surgery may pose a higher risk of complications.
- Patients seeking a non-invasive option to avoid surgery-related risks and toxicity, such as bleeding, infection, or long recovery times. Excellent results and low toxicities support this therapeutic option.
- Recurrent tumors (even after radiation treatment) where surgery is not feasible or has already been performed.
- Functional disorders such as trigeminal neuralgia, where CyberKnife can precisely target affected nerves without invasive procedures.
Case in Point: CyberKnife vs. Prostatectomy for Prostate Cancer
Prostatectomy (surgical removal of the prostate) has been a standard treatment for prostate cancer, but CyberKnife stereotactic body radiation therapy (SBRT) presents a compelling alternative.
Key Differences
- CyberKnife is completely non-invasive, whereas prostatectomy requires surgery with potential risks like bleeding and infection.
- CyberKnife targets the tumor with sub-millimeter accuracy, sparing nearby healthy tissue, including the bladder, urethra, and rectum.
- Prostatectomy can lead to issues such as urinary incontinence and erectile dysfunction, while CyberKnife minimizes damage to nearby nerves and reduces these risks.
- Surgery requires hospital stays and weeks of recovery, whereas CyberKnife is an outpatient procedure with no downtime.
- Prostatectomy is a single procedure with a recovery period, while CyberKnife typically requires five or fewer sessions, each lasting 30 minutes.
In early-stage prostate cancer or for those seeking a less disruptive treatment option, CyberKnife can be an effective, safe, and convenient first option for treatment.
Key Benefits of CyberKnife
To summarize, the advantages associated with CyberKnife are as follows:
- Non-invasive: No surgery or anesthesia required.
- High precision: Targets tumors with extreme accuracy.
- Real-time tumor tracking: Adjusts for movement, ensuring consistent radiation delivery.
- Versatile: Effective for tumors in the brain, spine, lung, liver, pancreas, prostate, lymph nodes, head and neck, adrenal gland, and kidney. Indicated for some pediatric tumors.
- Shorter treatment times: Fewer sessions than conventional radiation therapy.
- Outpatient procedure: No hospital stay is needed, allowing a quick return to daily activities.
- Reduced side effects: Minimal damage to surrounding healthy tissues.
- Re-Treatment After Previous Radiation: CyberKnife enables safe re-treatment for select tumors, depending on prior exposure and tumor location.
CyberKnife offers patients a personalized and potentially more comfortable radiation therapy experience.
Conditions Treated
Prostate Cancer
CyberKnife reduces treatment-related side effects such as incontinence and erectile dysfunction. Studies show that 5-year disease-free survival rates range from 93-98% in low and intermediate risk groups. Side effects may include temporary urinary irritation and mild bowel changes. It is also an option for recurrent prostate cancer after prior radiation.
Lung Cancer (Primary and Metastatic)
CyberKnife has been shown to be effective for early-stage NSCLC and lung metastases, especially for non-surgical candidates. Real-time tracking compensates for breathing motion, reducing exposed healthy lung tissue and achieving local tumor control rates of 85-90%. Side effects may include mild lung inflammation (radiation pneumonitis), cough, and fatigue.
Brain Tumors and Metastases
Used for benign (meningiomas, schwannomas) and malignant tumors (ependymomas, gliomas) and metastases. CyberKnife preserves healthy brain tissue while achieving 80-90% tumor control. Possible side effects include temporary headaches, mild swelling, or transient neurological symptoms.
Breast Cancer
A non-invasive alternative for early-stage and recurrent breast cancer. Studies into partial breast irradiation suggest high tumor control rates with fewer side effects than whole-breast radiation. Some patients may experience mild skin irritation, swelling, or fatigue.
Liver Cancer (Primary and Metastatic)
Effective for HCC and liver metastases, especially in non-surgical candidates. It preserves liver function while maintaining 80-90% tumor control rates. Side effects include temporary liver enzyme elevation and mild nausea.
Spinal Tumors
Treats spinal metastases, chordomas, and benign tumors without invasive immobilization. Control rates exceed 85-90%. Some patients may experience temporary pain flare-ups or mild spinal cord irritation.
Pancreatic Cancer
Provides a treatment option for locally advanced pancreatic cancer, improving survival in select cases where the tumor is favorably located, and motion management allows safe delivery of ablative radiation doses near sensitive gastrointestinal structures. Side effects may include mild nausea and temporary digestive issues.
Kidney Cancer
A non-invasive alternative for kidney cancer, with promising early results.
Non-Cancerous Conditions
Trigeminal Neuralgia
CyberKnife offers a non-surgical approach, delivering targeted radiation to the nerve. Studies indicate that 70-85% of patients experience significant pain relief. Potential side effects may include mild numbness or tingling sensations.
Arteriovenous Malformations (AVMs)
Radiation gradually closes abnormal blood vessels, reducing bleeding risk. Up to 80% obliteration can occur within 1-3 years. Temporary headaches or mild swelling may occur.
Acoustic Neuroma
An effective alternative to surgery, better preserving hearing and balance in many cases. Over 90% tumor control rates are reported, with occasional dizziness or slight hearing loss.
Who is a Candidate for CyberKnife?
CyberKnife is suitable for patients with various cancers and non-cancerous conditions, especially those who are not candidates for surgery or are seeking a non-invasive treatment option. Eligibility depends on multiple factors that necessitate a thorough evaluation by a radiation oncologist.
Criteria for Eligibility
- Cancer Type: CyberKnife is effective for both benign and malignant tumors, including those located in the brain, lungs, prostate, spine, liver, pancreas, and kidneys. It is ideal for early-stage cancers or localized tumors that have not spread extensively. It is also indicated for the treatment of metastases, having a potentially curative purpose in patients with limited metastases, known as an oligometastatic state.
- Tumor Size: Smaller tumors are better suited for CyberKnife. Treatment is typically most effective for tumors up to 6 cm in size. The efficacy of CyberKnife for treating larger tumors is under active research, with some studies showing promising results through fractionated dosing.
- Location: The tumor's location is crucial. CyberKnife is ideal for tumors in hard-to-reach places or near sensitive structures where traditional surgery might not be feasible. However, some tumors that are surgically accessible can be treated just as effectively with CyberKnife, without the inconveniences and side effects of surgery.
- Health Status: Patients who are medically frail or have contraindications to surgery (e.g., due to age, comorbidities) may benefit from CyberKnife due to its non-invasive nature and precision.
When is CyberKnife Not Recommended?
CyberKnife may not be recommended in all cases, and this determination is made through careful assessment by a multidisciplinary team during weekly tumor committee meetings. These collaborative sessions are dedicated to reviewing each case in detail to evaluate the most appropriate radiotherapy strategy, considering whether CyberKnife is suitable, and also discussing the potential integration of other cancer therapies. Recommendations extend to the optimal sequencing of treatments to enhance overall effectiveness and patient outcomes.
Large Tumor Size and Location: Tumor size is considered while evaluating candidacy, with small tumors given preference. However, emerging research and clinical trials suggest that the technology may be feasible in select cases involving larger tumors (over 5 cm) with careful planning. The location of the tumor is another crucial factor. Doctors will consider aspects such as proximity to critical organs in the decision-making process.
The advanced CyberKnife M6 system has been shown to be capable of treating larger tumors with enhanced precision. However, the decision to proceed with CyberKnife therapy depends on an assessment involving specialists in Radiation Oncology and Medical Physics, who rely on current scientific evidence and clinical experience to guide treatment planning.
CyberKnife Treatment Procedure
Planning and Preparation
Before treatment, patients undergo a detailed treatment planning session using imaging technology (CT, MRI, PET, angiography) to map the tumor’s location precisely. A customized mask or immobilization device may be used to hold the patient still during treatment, especially for head and neck tumors.
Treatment Session
The CyberKnife procedure is performed in an outpatient setting. The patient lies on a treatment table, and the robotic arm delivers precise radiation beams from different angles, guided by real-time imaging. Sessions usually take between 15 minutes to 1 hour, depending on tumor complexity and the number of targets to be treated in the same session.
Is CyberKnife Treatment Painful?
The treatment is painless. There is no discomfort during the radiation delivery, and most patients experience little to no pain after the procedure.
Recovery
Post-Treatment Care
Patients can typically resume normal activities after treatment, though they may experience temporary fatigue or mild swelling. Follow-up appointments are set up to monitor recovery and assess treatment efficacy.
How Long Does it Take for CyberKnife to Work?
Following Cyberknife treatment, tumor shrinkage or symptom relief may take weeks to months, depending on the condition being treated.
Potential Side Effects and Complications
Common Side Effects
- Fatigue: This is one of the most common post-treatment side effects.
- Temporary swelling: This is particularly possible in brain or head/neck treatments.
- Nausea: Reported with treatments targeting abdominal or pelvic tumors, although it is exceedingly rare.
Complications
Although CyberKnife is a non-invasive procedure, complications may include:
- Temporary pain flare-ups or inflammation at the treatment site.
- Nerve damage, although rare, may occur in cases of spine or brain tumor treatments.
Latest Research and Advancements
Research is ongoing to expand CyberKnife’s applications, including its potential use in neurological conditions like Parkinson’s disease, epilepsy, and OCD. Early trials suggest positive results, and CyberKnife is being explored as a treatment for movement disorders owing to its precision and capacity to target specific regions of the brain.
Recent advancements in imaging technology and motion management have improved CyberKnife’s precision, enabling better outcomes for tumors that move. Innovations in robotic systems also enhance treatment speed and accuracy, further shortening the duration of sessions.
Conclusion
Advances in radiotherapy have significantly broadened the range of treatment options available for cancer and other conditions, improving precision and patient outcomes. CyberKnife represents one of several modern tools developed to deliver targeted, non-invasive radiation therapy. While it offers potential advantages in select cases - particularly for patients who are not candidates for surgery - its use depends on individual clinical considerations. As technology and research continue to evolve, systems like CyberKnife may play an increasingly important role in multidisciplinary treatment planning.

Dr. Aurora Rodríguez is the Head of the Radiation Oncology Department at Hospital Ruber Internacional from Quirónsalud Hospital Group and a leading expert in advanced radiotherapy techniques with over 25 years of experience. She is a former General Secretary of the Spanish Society of Radiation Oncology and currently coordinates its Interdisciplinary Patient Platform. Dr. Rodríguez has an extensive academic background, has led multiple clinical trials, and is widely recognized for her contributions to cancer research and patient-centered radiotherapy care.

Dr. Rafael García is a senior radiation oncologist at Hospital Ruber Internacional from Quirónsalud Hospital Group, specializing in central nervous system and urological tumors. With over two decades of experience and leadership in radiosurgery and SBRT, he also serves as the National Coordinator of the Radiosurgery/SBRT Group of the Spanish Society of Radiation Oncology. He is actively involved in clinical research and teaching, with numerous publications and contributions to national and international oncology conferences.

Hospital Ruber Internacional from Quirónsalud Hospital Group is a leading private hospital in Madrid, Spain, known for its top specialists, advanced technology, focus on innovation, and commitment to continual advancement in healthcare. The hospital offers cutting-edge treatments in various specialties, such as cancer, cardiovascular, and neurological conditions.
The addition of the latest Da Vinci robotic system model "xi" has further enhanced surgical precision and expanded treatment capabilities across various specialties, establishing Hospital Ruber Internacional's position as a global leader in healthcare innovation and patient care.
References:
Featured Blogs



