When Does a Hematoma Need to Be Drained?

Medically Reviewed and Updated by Dr. Sony Sherpa, (MBBS) - July 30, 2024
Overview
A hematoma refers to a pooling of blood in the surrounding tissues after an injury to the blood vessels. An injury to small blood vessels is called a bruise, whereas if larger blood vessels are involved, it is termed a hematoma. A hematoma is generally associated with pain and swelling. Injuries occurring in capillaries, veins, or arteries can form hematomas.
The difference between a hematoma and a hemorrhage is that the latter refers to persistent bleeding, whereas the former typically has already formed a clot. A hematoma can arise from injuries, certain medications such as aspirin, clopidogrel, warfarin, rivaroxaban, dabigatran, and bleeding disorders such as thrombocytopenia.
Most hematomas are harmless and not a cause for concern. They usually resolve over time as the blood clot is removed and the blood vessels are repaired. However, some hematomas need surgical drainage depending on the location and symptoms.
Types of Hematoma
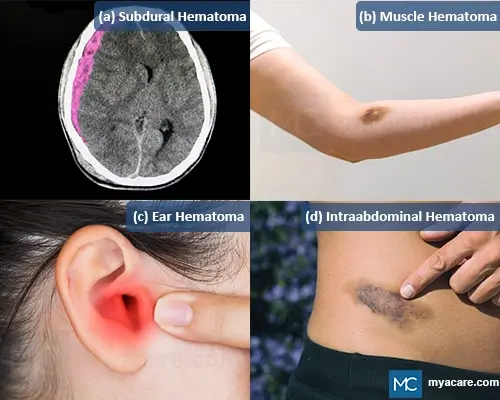
Hematomas are classified and named based on their location in the body. The severity and need for surgical drainage are also primarily based on the location of the hematoma. A few examples of hematomas include:
- Epidural hematoma: A collection of blood between the skull and the dura mater (the outer protective lining of the brain).
- Subdural hematoma: It is the collection of blood between the dura mater and the arachnoid mater (lining of the brain that lies deeper than the dura mater).
- Muscular hematoma: It is a hematoma formed within the muscle group
- Ear hematoma: It occurs between the auricular cartilage and the perichondrium.
- Peritoneal hematoma: Hematoma formed within the peritoneum.
- Retroperitoneal hematoma: Hematoma formed in the retroperitoneal structures, posterior to the peritoneum.
- Intraabdominal hematoma: Hematoma formed within the abdomen.
- Splenic hematoma: It is a hematoma formed in the spleen.
- Hepatic hematoma: Hepatic hematomas are formed in the liver.
- Scalp hematoma: Hematoma formed within a layer of the scalp.
- Nasal septal hematoma: A septal hematoma is formed within the nasal septum, separating two nasal passages.
- Subcutaneous hematoma: Hematoma formed beneath the skin in the subcutaneous layer.
- Subchorionic hematoma: Hematoma formed beneath the placenta in intrauterine pregnancy.
Causes and Risk Factors for Hematoma
Understanding the causes and risk factors for hematoma formation can help in preventing and managing this condition:
- Trauma: Direct blows or injuries, such as falls, car accidents, or sports injuries, are common causes of hematomas. The impact can damage blood vessels, leading to blood leakage and hematoma formation.
- Aneurysm: An aneurysm, or a weakened blood vessel that bulges, can rupture and cause a hematoma. This is especially critical if it occurs in the brain, leading to a subdural or intracranial hematoma.
- Medication: Certain medications, especially anticoagulants (blood thinners) like warfarin, aspirin, or clopidogrel, increase the risk of bleeding and hematoma formation even with minor trauma.
- Fracture: Bone fractures can lead to the formation of hematomas as blood vessels are damaged during the injury. These hematomas often occur in conjunction with the fracture site.
- Surgical Procedures: Post-surgical hematomas can develop due to bleeding from the surgical site. This is a common complication that may require drainage to prevent infection and facilitate healing.
Signs and Symptoms of Hematoma
Recognizing the signs and symptoms of a hematoma is crucial for timely diagnosis and treatment:
Signs of Hematoma
- What Does a Hematoma Look Like? Hematomas often appear as a raised, swollen area under the skin. They can vary in color from dark red to purple, blue, or even black as the blood beneath the skin ages. Over time, the hematoma may change colors, similar to a bruise, but it typically remains more pronounced and raised.
- Bruising with a Lump: Unlike regular bruises, hematomas often present as a palpable lump beneath the skin. This lump can be firm to the touch and may vary in size depending on the amount of blood that has pooled in the area.
Symptoms of Hematoma
- Pain and Tenderness: Hematomas are usually painful, especially when touched or pressed. Hematomas can cause a dull ache or sharp pain, depending on their size and location.
- Swelling and Inflammation: The area around the hematoma often becomes swollen and inflamed. This swelling can restrict movement if the hematoma is near a joint or in a muscle.
- Warmth and Redness: The skin over the hematoma may feel warm to the touch and appear red due to the body's inflammatory response to the injury.
- Reduced Mobility: Large hematomas, especially those in the muscles or near joints, can limit movement and function. This is especially noticeable in the limbs, where swelling and pain can make walking or using an arm quite difficult.
- Headache and Confusion: In cases of intracranial hematomas, symptoms may include headache, confusion, dizziness, and other neurological signs, indicating increased intracranial pressure.
Treatment for Hematoma
The treatment of hematoma depends on the location, symptoms, and medical condition of the patient. Most hematomas require no specific treatment and resolve on their own. However, sometimes they can be a medical emergency requiring prompt treatment.
Even if the hematoma resolves on its own, self-care is important to prevent complications and reduce pain and swelling.
The following steps can be carried out to care for hematoma at home. These steps can be remembered with the acronym RICE.
- Rest.
- Ice: apply an ice pack or compression for 20 minutes at a time for 48 hours following the injury to reduce swelling and inflammation.
- Compression: Light compression is helpful by wrapping the area with an elastic bandage.
- Elevation: Elevation of the injured area above the level of the heart is recommended.
- Additionally, you can take pain medications such as acetaminophen. However, do not consume other pain medications like aspirin or ibuprofen on your own, as they can slow the clotting process and increase the risk of bleeding.
Surgical Drainage
In certain situations, hematomas require surgical drainage. It depends on the location of the hematoma and the severity of the symptoms. It also dictates the type of procedure and its urgency.
Certain indications for surgical drainage of hematoma are mentioned below:
1. Epidural Hematoma: This type of hematoma is generally due to arterial bleeding between the skull plate and the outer lining of the brain. The cause of epidural hematoma is almost always traumatic.
Urgent surgical hematoma evacuation is required for the patient with large extradural hematoma, i.e., >30 ml or causing a focal or progressive neurological deficit. This is particularly important to prevent brain death caused by increased pressure inside the brain. The evacuation of the hematoma is done by a neurosurgeon.
Other indications for surgical evacuation include cases of coma or showing early signs of brain herniation in imaging.
Other patients with smaller epidural hematomas can be managed conservatively by close observation and by preventing complications.
2. Subdural hematoma: Subdural hematoma is generally the tearing of veins in the space between the internal linings of the brain. It is a neurological emergency that may cause irreversible brain damage and death. So, they must be evaluated for surgical drainage immediately. A clinical examination and brain imaging are required for assessment.
Most subdural hematomas can be managed conservatively. A study done in 2015 on people with subdural hematomas showed that the majority received conservative treatment. Only 6.5% of these study participants required surgical drainage later in life.
The following are the clinical indications for surgical drainage of subdural hematoma:
- Subdural hematoma with >10 mm of maximal thickness in imaging
- Imaging shows brainstem compression or >5mm of midline shift
- Hematoma causing drowsiness or dilated pupils
- The patient continues to deteriorate clinically
Patients who do not fulfil the above criteria for surgical drainage should be monitored regularly for at least 24 hours. The surgical drainage is done by a neurosurgeon.
3. Muscle hematoma: Muscle hematoma is due to the extravasation of blood in the muscle group. They can be spontaneous or traumatic. Generally, traumatic hematomas are managed conservatively and resolve on their own. However, there is a risk of ongoing bleeding in spontaneous hematoma that can be life-threatening. So, the bleeding vessel must be identified using a CT angiogram.
Surgical evacuation of muscular hematoma is indicated when there is a neurological compromise due to the hematoma or localized ischemia. Surgical evacuation is usually performed by a general surgeon or an orthopedic or trauma surgeon. Arterial embolization is also considered a treatment option for muscular hematoma.
4. Auricular hematoma: Auricular hematoma forms in the auricle due to direct trauma. Every auricular hematoma must be drained. If not drained, it can disrupt the blood supply to the auricular cartilage, causing necrosis.
In patients with hematomas less than 2 cms in diameter and presenting within 48 hours, needle aspiration is suggested.
Incision and drainage are suggested for larger hematomas more than 2 cms in diameter or those presenting after 48 hours. The evacuation for auricular hematoma is done by an ENT surgeon
5. Subungal hematoma: It is a hematoma under a fingernail or toenail. Trephination is the process of placing one or more holes in the nail to permit the drainage of blood. It is indicated if the hematoma is acute, not spontaneously draining, with intact nail folds, and painful. The procedure is not effective after 48 hours. Trephination can be done by electrocautery, laser, syringe, or nail puncture.
6. Lower limb hematoma: A hematoma on the shin is usually treated by surgical drainage. Other hematomas on the lower leg are mostly treated conservatively. Similarly, a large hematoma that does not improve over a week usually requires surgical drainage.
Comparing a Hematoma and Bruise/Contusion
Understanding the differences between a hematoma and a bruise (contusion) is essential for proper diagnosis and treatment:
- Hematoma: A hematoma is a localized collection of blood outside the blood vessels, usually resulting from trauma or injury that causes a blood vessel to rupture. Hematomas can vary in size and severity, often appearing as a raised, swollen area with a dark red or purplish coloration. They are typically more severe than bruises and may require medical intervention if they cause significant pain, pressure on vital structures, or risk of infection.
- Bruise/Contusion: A bruise, or contusion, is a common injury where small blood vessels under the skin break due to trauma, causing blood to leak into the surrounding tissues. Bruises are usually less severe than hematomas and appear as flat, discolored areas on the skin, typically changing color from red to purple, green, and yellow as they heal. Bruises generally heal on their own without medical intervention, although severe bruising may require evaluation to rule out underlying issues.

Common Indications for Hematoma Drainage
Hematoma drainage is indicated in various clinical situations to prevent complications and improve patient outcomes. Common indications include:
- Pressure on Vital Structures: When a hematoma exerts significant pressure on the spinal cord, brain, or other vital organs, drainage is essential. For instance, expanding cranial hematomas can increase intracranial pressure, leading to potential brain damage if not promptly addressed. Spinal hematomas can compress the spinal cord, causing neurological deficits that may become permanent without timely intervention.
- Risk of Infection: Hematomas, particularly large ones or those located in regions prone to bacterial contamination, pose a significant risk of infection. Draining the hematoma helps prevent the development of abscesses, which can complicate the patient’s condition and lead to severe systemic infections.
- Pain and Discomfort: Persistent or severe pain associated with a hematoma may necessitate drainage to alleviate discomfort and improve mobility.
- Delayed Healing: Hematomas that impede healing processes, especially in post-surgical or trauma patients, may require drainage to facilitate recovery and prevent further complications.
- Compartment Syndrome: In cases where a hematoma leads to increased pressure within a confined anatomical space, such as a limb compartment, urgent drainage is needed to prevent tissue damage and loss of function.
Techniques Used for Hematoma Drainage
Various techniques are employed for hematoma drainage, each suited to different clinical scenarios and patient needs:
- Surgical Procedures: Surgical drainage involves making an incision over the hematoma site to evacuate the accumulated blood. This method is typically used for large hematomas or those located in critical areas where precise control and thorough evacuation are necessary. It is often performed under general or local anesthesia, depending on the hematoma's location and size.
- Percutaneous Drainage: This minimally invasive technique involves inserting a needle or catheter through the skin into the hematoma to aspirate the blood. Percutaneous drainage is usually guided by imaging techniques, such as CT or ultrasound, to ensure accurate placement. It is often used for accessible hematomas that do not require extensive surgical intervention.
- Ultrasound-Guided Drainage: Ultrasound guidance enhances the precision of percutaneous drainage, particularly for hematomas located in deeper tissues or near vital structures. Ultrasound's real-time visuals guide clinicians in precisely navigating needles or catheters, reducing the risk of complications and enhancing the procedure's success.
Complications
If a hematoma is left untreated, it can sometimes result in various complications. Complications also vary according to the site.
- Hematoma in the brain can permanently damage brain cells leading to loss of brain function in the part involved.
- Auricular hematoma, if untreated, can lead to the death of auricular cartilage.
- Nasal septal hematoma has a high risk of forming an abscess and can lead to sepsis.
- Muscle hematoma can undergo a reactive process resulting in myositis ossificans, in which muscle loses its function and elasticity.
Frequently Asked Questions
How long does it take for a hematoma to heal?
The healing time for a hematoma varies depending on its size, location, and the individual's overall health. Minor hematomas often resolve within a few days to a couple of weeks. Larger or deeper hematomas may take several weeks to a few months to fully heal. Proper rest, elevation, and avoiding strenuous activities can help speed up the healing process. In cases where surgical or percutaneous drainage is performed, the recovery period may be shorter, but it still requires adequate follow-up and care.
How do you tell if a bruise is a hematoma?
To determine if a bruise is actually a hematoma, observe the following signs: hematomas are typically larger, more swollen, and more painful than bruises. They often form raised, firm lumps, whereas bruises are usually flat and less severe. Hematomas may also result from more significant trauma and can take longer to heal, sometimes requiring medical intervention.
Is a hematoma dangerous in the leg?
A hematoma in the leg can be dangerous depending on its size, location, and underlying cause. While small hematomas often resolve on their own without complications, larger hematomas can cause significant pain, swelling, and pressure on surrounding tissues. If left untreated, they may lead to complications such as infection, impaired blood flow, or compartment syndrome, a serious condition where increased pressure within the muscles can damage nerves and blood vessels.
When to Call A Doctor
It is important to seek medical attention for a hematoma under certain conditions to prevent complications and ensure proper healing:
- Severe Pain: If you experience significant pain from a hematoma or if over-the-counter pain relievers do not help, it is best to see a doctor for evaluation.Increasing Size: A hematoma that continues to grow in size or swelling should be evaluated to determine if drainage or other interventions are necessary.
- Restricted Movement: Difficulty moving the affected limb or joint due to a hematoma may require medical evaluation.
- Signs of Infection: Redness, warmth, increased swelling, and fever are signs of infection that need prompt medical attention.
- Head Injury Symptoms: In cases of head trauma, symptoms like headache, confusion, dizziness, or loss of consciousness warrant immediate medical evaluation to rule out intracranial hematomas.
- Underlying Conditions: Individuals on blood thinners or those with bleeding disorders should seek medical advice if they develop a hematoma, even if it appears minor.
Final Takeaway
Hematoma is the accumulation of blood in the surrounding tissues following an injury to blood vessels. Most hematomas resolve on their own. However, adequate care is required to avoid complications.
The requirement for surgical drainage of hematoma varies according to the location and severity of the hematoma. Those who have head injuries, ear injuries, or show signs of infection such as discoloration, swelling, and a localized rise in temperature, should seek urgent medical care. If the condition is identified in time and with appropriate intervention, complications are unlikely.
To search for the best Neurology Healthcare Providers in Croatia, Germany, India, Malaysia, Spain, Thailand, Turkey, Ukraine, the UAE, UK and the USA, please use the Mya Care search engine.
To search for the best healthcare providers worldwide, please use the Mya Care search engine.
The Mya Care Editorial Team comprises medical doctors and qualified professionals with a background in healthcare, dedicated to delivering trustworthy, evidence-based health content.
Our team draws on authoritative sources, including systematic reviews published in top-tier medical journals, the latest academic and professional books by renowned experts, and official guidelines from authoritative global health organizations. This rigorous process ensures every article reflects current medical standards and is regularly updated to include the latest healthcare insights.

Dr. Sony Sherpa completed her MBBS at Guangzhou Medical University, China. She is a resident doctor, researcher, and medical writer who believes in the importance of accessible, quality healthcare for everyone. Her work in the healthcare field is focused on improving the well-being of individuals and communities, ensuring they receive the necessary care and support for a healthy and fulfilling life.



