Embryo Selection in IVF: Clinical Approaches and Evidence-Based Techniques
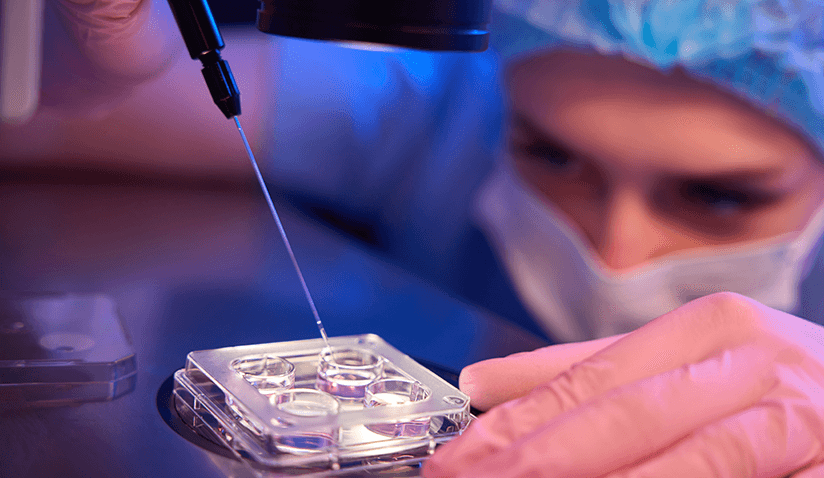
Embryo selection is a crucial step in assisted reproductive treatment (ART), specifically in IVF (in vitro fertilization), identifying the most viable embryos for transfer through careful selection for achieving a successful pregnancy. This process involves evaluating embryos based on their morphological characteristics, genetic health, and developmental potential to enhance the likelihood of implantation and healthy birth.
The primary goal of embryo selection is to identify the healthiest embryos, reducing the risk of miscarriage and genetic abnormalities while improving overall IVF success rates. Advances in reproductive medicine, including preimplantation genetic testing (PGT) and time-lapse imaging, have refined this selection process, allowing embryologists to make more informed decisions.
Embryology plays a central role in IVF, as embryologists analyze and nurture fertilized eggs in a controlled laboratory environment. Their expertise in assessing embryo quality, optimizing culture conditions, and applying selection techniques is essential in determining the best embryos for transfer, ultimately improving pregnancy outcomes.
The IVF Process and Embryo Development
IVF is a multi-step assisted reproductive technology involving several key stages that lead to embryo development:
- Ovarian Stimulation – Using hormonal medications, the ovaries are stimulated to produce multiple mature eggs, which significantly increases the potential for obtaining viable embryos.
- Egg Retrieval – Mature eggs are collected via follicular aspiration, a minimally invasive procedure performed under ultrasound guidance.
- Fertilization – In the laboratory, retrieved eggs are fertilized with sperm. Fertilization occurs through either conventional IVF, by combining sperm and eggs in a dish, or intracytoplasmic sperm injection (ICSI), by injecting a single sperm directly into an egg.
- Embryo Culture – The fertilized eggs, now called embryos, are cultured for several days in a controlled environment, allowing embryologists to monitor their development before selection for transfer.
Stages of Embryo Development
After fertilization, the embryo progresses through several developmental stages:
- Zygote (Day 1) – A single-cell fertilized egg containing genetic material from both parents.
- Cleavage Stage (Days 2–3) – Rapid cell division forms a multicellular embryo within the zona pellucida (protective shell).
- Morula (Day 4) – The embryo reaches approximately 16–32 cells, resembling a solid ball, as it continues dividing. The morula stage marks a critical transition before forming a blastocyst, with cells compacting and beginning differentiation.
- Blastocyst (Days 5–6) – A fluid-filled cavity forms, with cells differentiating into the inner cell mass (which becomes the fetus) and the trophoblast (which forms the placenta). Blastocysts generally have a higher implantation potential compared to earlier-stage embryos. However, embryo transfer timing may vary based on patient-specific factors and lab protocols.
Each developmental stage is crucial for embryo viability, and advanced selection methods help identify optimal embryos for transfer, enhancing the chances of pregnancy.
Embryo Grading
Following fertilization, embryos are graded based on:
- Expansion stage (blastocyst development).
- Inner cell mass quality (future fetus potential).
- Trophectoderm quality (future placenta development).
Factors That May Affect Embryo Quality
The quality of an embryo is influenced by multiple factors, including maternal and paternal health, sperm selection techniques, and strategies to improve gamete integrity.
Maternal Factors
Embryo quality is significantly affected by maternal age. This decline is largely attributed to chromosomal abnormalities and mitochondrial dysfunction in aging eggs. Other maternal influences include:
- Ovarian Reserve – A diminished ovarian reserve reduces the number of high-quality eggs available for fertilization.
- Metabolic and Hormonal Health – Conditions like polycystic ovary syndrome (PCOS), obesity, and insulin resistance can impair egg quality and embryo development.
- Lifestyle Factors – Oocyte quality is adversely affected by smoking, excessive alcohol intake, and poor nutrition.
Paternal Factors
Sperm quality plays a critical role in embryo development, as sperm DNA integrity affects fertilization and early embryonic growth. Factors that influence sperm quality include:
- Age and Oxidative Stress – Advanced paternal age is associated with increased sperm DNA fragmentation and reduced fertilization potential.
- Lifestyle and Environmental Exposures – Smoking, poor diet, and exposure to toxins can contribute to sperm damage.
- Underlying Medical Conditions – Conditions such as varicocele, infections, and hormonal imbalances can impair sperm function.
Sperm Selection and Steps to Improve Quality
Optimizing sperm quality is essential for embryo viability. To ensure optimal fertilization, techniques like intracytoplasmic morphologically selected sperm injection (ICSI) and microfluidic sperm sorting are used to identify and select the most viable sperm.
Research-Backed Approaches to Improve Sperm Quality
- Local Renin-Angiotensin System and Sperm DNA Fragmentation – The renin-angiotensin system (RAS) is a hormone system involved in regulating blood pressure and fluid balance in the body. Beyond its role in circulation, a local renin-angiotensin system (local RAS) exists in various tissues, including the testes, where it influences sperm development and function. Emerging research suggests that targeting the local RAS in the testes can help improve sperm quality by reducing oxidative stress and DNA damage, which are key factors affecting male fertility. By modulating this system, scientists aim to enhance sperm health, motility, and overall fertilization potential, offering a promising approach to improving male reproductive outcomes.
- Oral Supplementation and DNA Repair Pathways – Studies show that oral supplementation with antioxidants, vitamins, and key nutrients targeting the ataxia-telangiectasia-mutated (ATM) repair pathway may help enhance sperm quality by reducing DNA damage. The ATM repair pathway plays a crucial role in detecting and repairing DNA breaks, ensuring genetic stability in sperm cells. By enhancing this repair mechanism, supplementation may support sperm integrity, motility, and overall fertility outcomes.
Enhancing both egg and sperm quality before IVF can greatly improve embryo viability and the likelihood of a successful pregnancy.
Embryo Selection Techniques
Various techniques help embryologists identify the most viable embryos for implantation, ensuring the best possible outcomes for prospective parents.
Morphological Assessment
Morphological assessment is one of the primary methods embryologists use to evaluate embryo quality. This involves examining:
- Cell Number: Healthy cleavage-stage embryos typically have 4 cells on day 2 and 6 to 8 cells on day 3.
- Symmetry: Evenly sized cells indicate normal development, while asymmetry may suggest impaired growth.
- Fragmentation: Fragments (small cell pieces) can reduce embryo viability. Embryos with minimal fragmentation have higher implantation potential.
Limitations of Morphology Alone
While morphological grading provides useful insights, it does not detect genetic abnormalities. Many embryos that appear normal may still have chromosomal errors, reducing their chances of implantation or leading to miscarriage. Advanced genetic testing techniques are used to improve selection accuracy.
Preimplantation Genetic Testing (PGT)
PGT enhances embryo selection by identifying chromosomal and genetic abnormalities before implantation. It helps determine whether embryos are normal, abnormal, or mosaic.
What is a Mosaic Embryo?
A mosaic embryo contains both normal and abnormal cells. These embryos may still have implantation potential, depending on the level of mosaicism. A low-level mosaic embryo has a small percentage of abnormal cells and may develop into a healthy baby (research shows comparable live birth rates to euploid embryos), while a high-level mosaic embryo contains more abnormal cells, increasing the risk of implantation failure or miscarriage. In both cases, genetic counseling is recommended.
PGT-A (Aneuploidy Testing)
PGT-A screens embryos for chromosomal abnormalities (aneuploidy) that can lead to implantation failure or miscarriage. It has significantly improved embryo selection, with clinical data showing that PGT-A achieves a blastocyst rate of 61%, an ongoing pregnancy rate per transfer of 61.5%, and a live birth rate of 54%. It is recommended for:
- Women over 35, since the risk of chromosomal errors increases with maternal age.
- Couples with recurrent pregnancy loss.
- Those with previous failed IVF cycles.
Method: A small sample of cells is taken from the embryo (trophectoderm biopsy) and analyzed using techniques like array comparative genomic hybridization (aCGH) or next-generation sequencing (NGS), with NGS being the more sensitive and specific method.
Benefits:
- Reduces miscarriage risk by transferring only chromosomally normal embryos.
- Improves implantation rates, leading to higher IVF success.
Non-invasive PGT-A (niPGT-A): Recent advances allow chromosomal analysis without embryo biopsy, using DNA fragments released into the culture medium. It may be noted that niPGT-A is a developing technique, which, while promising, requires further research to validate its accuracy compared to standard PGT. It is not a diagnostic technique but rather a method used to genetically prioritize embryos for transfer.
STAR Trial: The Single Embryo Transfer of Euploid Embryo (STAR) trial confirmed that selecting normal embryos significantly improves live birth rates.
PGT-M (Monogenic/Single Gene Defects)
PGT-M is used when couples carry a known genetic mutation that could be passed to their child. It screens for conditions like:
- Cystic fibrosis
- Huntington's disease
- Sickle cell anemia
- Fragile-X syndrome
Method: Polymerase chain reaction (PCR) is used to amplify and detect the specific mutation.
Benefits:
- Ensures that only embryos free of the targeted disease are transferred.
- Significantly reduces the risk of transmitting inherited genetic disorders.
PGT-SR (Structural Rearrangements)
PGT-SR detects structural chromosome abnormalities such as:
- Robertsonian translocations
- Reciprocal translocations
- Inversions
Method: To detect chromosomal imbalances, a biopsy of the trophectoderm (outer layer of the blastocyst) is performed, and the sample is analyzed using next-generation sequencing.
Benefits:
- Identifies embryos with balanced chromosomal structures, reducing the risk of implantation failure.
- Helps prevent complications from translocations or inversions in chromosomes.
- Assists couples with recurrent pregnancy loss or a history of structural chromosome disorders.
- Supports individuals with known chromosomal rearrangements in achieving a successful pregnancy.
Time-Lapse Imaging
Time-lapse imaging continuously monitors embryo development without disturbing their culture environment. Incubators capture thousands of images, allowing embryologists to track cell division patterns and identify embryos with the best developmental potential.
Benefits:
- Enhances embryo selection accuracy.
- Reduces handling stress, maintaining optimal culture conditions.
Cryopreservation and Egg Donation: Expanded Avenues for Embryo Selection
In addition to fresh embryo transfers, many IVF cycles involve the use of cryopreserved embryos or donor eggs - approaches that can significantly impact embryo selection and treatment outcomes.
Cryopreservation enables the storage and future use of high-quality embryos, often allowing patients to undergo frozen embryo transfers (FETs) without repeating ovarian stimulation. When embryos are carefully selected and vitrified at the blastocyst stage, clinical outcomes can be highly favorable. Data from high-performing fertility clinics suggest that cryotransfers are associated with a pregnancy rate of approximately 64% and a live birth rate of around 55%. However, these outcomes can vary depending on factors such as embryo quality, endometrial receptivity, patient age, underlying infertility diagnosis, and the laboratory’s freezing and thawing protocols.
Egg donation offers another important avenue, especially for individuals with diminished ovarian reserve, advanced maternal age, or genetic conditions that may impact embryo viability. The use of carefully screened donor eggs allows embryo selection to focus on optimizing implantation potential, often through the transfer of a single high-quality embryo. Clinical data reported an average pregnancy rate of 69% and a live birth rate of about 54% in donor egg cycles. Still, these outcomes can vary and may be influenced by factors such as the recipient’s uterine environment and synchronization protocols.
Taken together, cryopreservation and egg donation expand the options for embryo selection and provide adaptable strategies aligned with each patient's reproductive goals and clinical profile.
Benefits of Embryo Selection
Summarizing aspects discussed above, here are some of the primary advantages of embryo selection. While these benefits are well-documented, individual outcomes may vary depending on broader health and fertility factors.
- Higher Implantation Rates
Selecting embryos with optimal morphology and chromosomal health improves implantation success.
- Reduced Miscarriage Risk
Screening reduces the transfer of embryos with chromosomal abnormalities, decreasing early pregnancy loss.
- Higher Likelihood of a Healthy Pregnancy
Choosing embryos with normal chromosomes enhances the chances of full-term pregnancy and lowers complications.
- Reduced Risk of Genetic Disorders
Preimplantation genetic diagnosis helps screen for structural chromosome abnormalities or mitochondrial disorders.
- Potentially Shorter Time to Pregnancy
Transferring the most viable embryos early may reduce the number of IVF cycles, easing emotional and financial strain.
Who Are Candidates for Embryo Selection?
Embryo selection is particularly beneficial for individuals and couples facing specific reproductive challenges, as discussed above. Considerations include:
- Advanced Maternal Age (Women over 35).
- Recurrent Pregnancy Loss.
- Family History of Genetic Disorders.
- Previous IVF Failures.
- Severe Male Factor Infertility.
Embryo selection, while highly effective, is not a guaranteed solution, and other factors, such as uterine health and overall maternal well-being, also play a role in IVF success.
Research and the Future of Embryo Selection
Ongoing research in embryo selection continues to refine techniques that improve IVF success rates while minimizing risks. Scientists are exploring new methods to enhance embryo viability assessment and increase the chances of a successful pregnancy.
Advancements in Selection Techniques
Emerging studies are focusing on refining how embryos are assessed for implantation potential. New approaches in imaging and time-lapse monitoring are being developed to improve the accuracy of embryo grading without invasive procedures.
Polygenic Embryo Screening (PES)
Polygenic screening is being explored as a way to assess embryos for complex genetic traits, such as disease risk or other inherited characteristics. While this approach holds promise, it also raises ethical concerns and technical challenges, as predicting future health outcomes based on multiple genes remains an evolving field.
Improvements in Genetic Testing
Ongoing research aims to make genetic testing methods more accurate and reliable. The goal is to reduce the risk of misdiagnosis while ensuring that viable embryos are not unnecessarily discarded. Advances in non-invasive testing techniques could allow for embryo assessment without the need for biopsies.
Artificial Intelligence and Embryo Selection
AI-based technologies are being integrated into fertility clinics to analyze large amounts of data from embryo imaging (assessing subtle morphological features invisible to the human eye) and genetic testing. These tools aim to enhance decision-making by predicting embryo viability with greater precision, potentially increasing implantation success rates.
Frequently Asked Questions (FAQs)
How do fertility specialists choose embryos for IVF?
Embryos are selected based on their development, appearance, and sometimes genetic testing results. Embryologists assess cell division patterns, symmetry, and genetic abnormalities to identify embryos with the highest implantation potential.
How do you know if an embryo is of good quality?
A high-quality embryo typically has an even number of cells, uniform size, and minimal fragmentation. Embryologists assess these characteristics under a microscope to identify the best candidates for transfer.
How accurate is genetic testing in embryo selection?
Genetic testing is highly accurate but not perfect. While it can detect many chromosomal abnormalities, there is still a small risk of misdiagnosis. Additionally, some conditions may not be detectable at the embryo stage.
Can genetic testing be performed on frozen embryos?
Yes, genetic testing can be done on embryos that have been frozen and thawed. However, the process requires careful handling to preserve embryo viability. Correct storage allows frozen embryos to remain viable for many years. The success of implantation depends on their initial quality and how well they withstand the freezing and thawing process.
What are the causes of poor embryonic quality?
Poor embryo quality can be due to genetic abnormalities, poor egg or sperm quality, suboptimal lab conditions, or underlying health conditions in the parents.
How many embryos are implanted in an IVF cycle?
Many clinics recommend a single embryo transfer (SET) to reduce the risks of multiple pregnancies. Furthermore, the practice of transferring the embryo at the blastocyst stage has gained traction based on recent research findings. However, in some cases, two embryos may be transferred, depending on the patient’s history and medical advice.
Can you get pregnant with poor-quality embryos?
Yes, although poor-quality embryos have lower implantation rates, some may still result in a successful pregnancy. The ability of an embryo to develop into a healthy baby depends on multiple factors, including uterine conditions and overall maternal health.

Dr. Jesús María Franco Iriarte is a senior embryologist specializing in molecular biology, human reproduction, and genetics, with a strong academic background that includes a PhD in Molecular Biology and various postgraduate degrees in genetics, biostatistics, and healthcare management. He is currently the Director of the assisted reproduction laboratory at Hospital Ruber Internacional from Quirónsalud Hospital Group in Madrid. His research focuses on sperm DNA fragmentation, cryopreservation, in vitro embryo selection, and PGTA, with numerous publications in renowned journals.
He is recognized for his contributions to assisted reproductive technologies (ART), including IVF, genetic counseling, and embryo genetic testing. He has worked internationally and actively participates in global conferences, holding leadership positions in organizations such as ASEBIR and SEF. He also offers cutting-edge treatments in fertility preservation and advanced reproductive procedures, providing personalized care for his patients.

Hospital Ruber Internacional from Quirónsalud Hospital Group is a leading private hospital in Madrid, Spain, known for its top specialists, advanced technology, focus on innovation, and commitment to continual advancement in healthcare. The hospital offers cutting-edge treatments in various specialties, such as cancer, cardiovascular, and neurological conditions. The addition of the latest Da Vinci robotic system model "xi" has further enhanced surgical precision and expanded treatment capabilities across various specialties, establishing Hospital Ruber Internacional's position as a global leader in healthcare innovation and patient care.
The center also houses one of the most advanced Assisted Reproduction Laboratories in Spain, featuring innovative techniques such as in vitro fertilization, egg vitrification, and preimplantation genetic diagnosis, led by renowned embryologists.
References:
Featured Blogs



