Hip Replacement: Advances in Arthroplasty, Recovery Protocols
Hip pain can greatly affect a person's mobility, independence, and quality of life. Whether caused by age-related wear and tear, arthritis, trauma, or underlying medical conditions, chronic hip discomfort often interferes with everyday activities like walking, climbing stairs, or even resting comfortably. Conservative treatments like medication, physiotherapy, or lifestyle changes often ease symptoms. However, if these are ineffective and pain becomes debilitating, hip replacement surgery may become a necessary and life-changing intervention.
Hip joint degeneration, often resulting from osteoarthritis, is the most common reason patients consider surgery. In a healthy hip, the ball-and-socket joint moves smoothly due to a cushion of cartilage and lubricating fluid. With degenerative changes, this cartilage wears away, leading to friction, stiffness, inflammation, and pain.
Historically, hip replacement was most commonly recommended for older adults in their late 60s or 70s. However, the landscape is rapidly changing. Today, people of all ages, including those in their 40s and 50s, are increasingly opting for surgery to maintain an active lifestyle, reduce dependency on pain medications, and regain independence. Advances in minimally invasive surgical techniques, real-time image guidance, implant materials, and postoperative rehabilitation have made hip replacements safer and more durable than ever, with many implants lasting 20 years or longer.
A well-indicated and properly implanted prosthesis can restore a patient’s quality of life, effectively addressing pain and functional limitations. Many patients regain the ability to walk effortlessly, climb stairs, travel, and even return to sports, which was once thought impossible. Following hip replacement and a proper post-surgical rehab program, individuals have gone on to resume actively participating in even high-impact activities, such as tennis, running, skiing, golf, or soccer.
What Is a Hip Replacement?
Hip replacement is a surgical approach to address severe hip joint damage. It is also known as hip arthroplasty. During the procedure, the affected joint is removed and replaced with a prosthetic component. The surgery is designed to ease discomfort, enhance joint mobility, and support a return to routine activities with less difficulty.
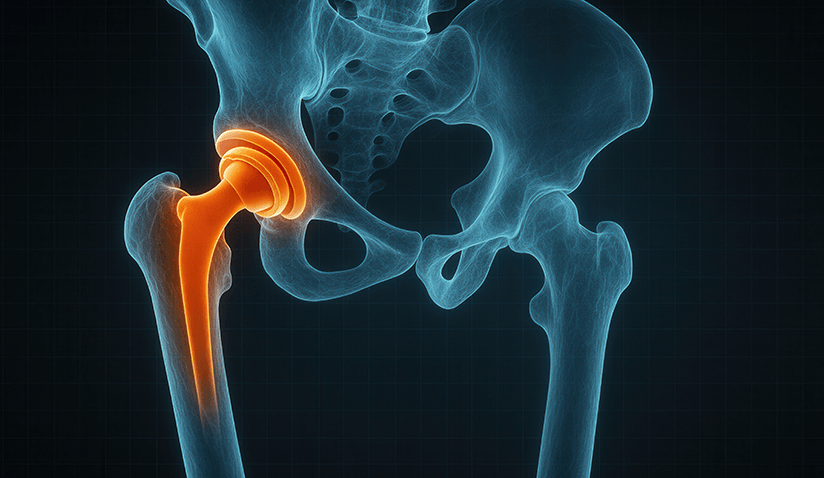
Components of a Hip Implant
The procedure involves replacing worn or damaged areas of the hip joint with prosthetic parts. These typically include:
- Femoral components - A ceramic or metal ball replaces the femoral head, supported by a metal stem placed into the femur (thigh bone).
- Acetabular component - A plastic, ceramic, or metal socket that replaces the damaged acetabulum.
- In some cases, a liner is placed inside the socket to ensure smooth movement between the ball and socket.
Materials Used
- Titanium or cobalt-chrome alloys: For the stem and socket.
- Ceramics: For low-wear articulation.
- Cross-linked polyethylene: Improves the wear resistance of liners.
Types of Hip Replacement Procedures
Hip replacement surgery is not a one-size-fits-all procedure. Depending on the patient’s age, diagnosis, bone health, and activity level, orthopedic surgeons may recommend one of several types of hip replacement. Each technique involves different components and degrees of joint replacement. The three main types are:
Total Hip Replacement (THR)
Also called total hip arthroplasty, this most commonly performed hip replacement procedure involves the surgeon removing and replacing both the femoral head and acetabulum with prosthetic parts.
Partial Hip Replacement (Hemiarthroplasty)
In this procedure, only the femoral head (ball) is replaced, while the natural socket is left intact. Hemiarthroplasty is mostly used to treat certain types of hip fractures, particularly displaced femoral neck fractures in elderly patients with lower activity levels.
This surgery is usually quicker, involves less bone removal, and is often sufficient when the acetabulum is healthy. However, it is less suitable for patients with arthritis, as it does not address socket wear or inflammation.
Hip Resurfacing
Rather than removing the entire femoral head, hip resurfacing involves trimming and capping it with a smooth metal covering. Similar to a THR, the socket is also fitted with a metal cup. This bone-conserving procedure is typically recommended for younger, active patients, especially men with strong bone quality and early-stage arthritis.
Hip resurfacing preserves more natural bone and allows for a greater range of motion, but it carries a higher risk of metal ion release and is not suitable for patients with osteoporosis or large femoral head deformities.
Advancements and Innovations in Hip Replacement Surgery
Minimally Invasive Techniques
Traditional surgical approaches use a relatively long incision, with extensive soft tissue exposure, to view and access the hip joint. Minimally invasive hip replacement, on the other hand, involves smaller incisions and muscle-sparing techniques to reduce tissue damage, and can be performed through either a single incision or two separate small incisions.
- Advantages: Reduced blood loss, shorter hospital stays, and quicker recovery times.
- Risks: May have a steeper learning curve for surgeons and potentially higher complication rates if not performed by experienced practitioners.
- Recovery: Many patients experience reduced pain after surgery and return to their daily tasks sooner.
Robot-Assisted and Navigation-Guided Surgery
Robot-assisted and navigation-guided methods are seeing broader application in hip replacement procedures. These systems use computer-generated 3D models, real-time imaging, and sensor feedback to help surgeons plan and execute highly precise implant placement. Compared to conventional surgery, navigation allows surgeons to tailor procedures for individual patients, adapting to their exact anatomy. For patients, this translates into greater safety, fewer complications, and improved functional outcomes in the medium and long term.
How It Works:
Before surgery, detailed imaging (such as CT scans) creates a virtual model of the patient’s hip. During surgery, robotic arms or navigation tools assist the surgeon through visual and tactile guidance. The system ensures accurate bone cuts and optimal positioning of the prosthetic components based on the preoperative plan.
Advantages:
- Greater Accuracy: Improved alignment and positioning of the implant reduces the risk of dislocation, uneven leg length, and wear.
- Consistency: Minimizes variability between surgeons and across procedures.
- Potential for Faster Recovery: More precise surgery may result in reduced soft tissue damage and faster functional recovery.
- Improved Longevity: Better implant positioning may extend the lifespan of the prosthesis, reducing the need for revision surgery.
Risks and Limitations:
- High Initial Costs: Robotic systems are expensive and may not be available in all hospitals.
- Learning Curve: Surgeons and teams require specific training to effectively use these systems.
- Ongoing Evaluation: While early data is promising, long-term outcomes are still under investigation.
Recovery:
Generally similar to traditional approaches, though patients may experience less postoperative pain and quicker rehabilitation due to enhanced surgical precision.
Recent Developments in Hip Replacement
- Outpatient hip replacement: Select patients can go home on the same day of surgery.
- Smart implants: Sensors monitor real-time data, such as load and temperature.
- Advanced materials: Use of more resistant alloys and high-density, cross-linked polyethylene and ceramic-on-polyethylene to reduce wear and prolong lifespan.
The contact surfaces of the artificial hip joint components have also improved significantly, which has helped increase the implant's useful life, allowing more young and active patients to undergo hip replacement with confidence.
Furthermore, the new generations of prostheses, tailored to each patient’s unique anatomy, allow for more natural integration with the bone, reduce the risk of loosening, and facilitate faster functional recovery, especially when combined with accelerated recovery protocols.
Advances in Recovery and Rehabilitation
Modern hip replacement recovery emphasizes early mobilization and reduced complication and re-admission rates through structured care pathways such as Enhanced Recovery After Surgery (ERAS) and Rapid Recovery Protocols. These are multidisciplinary, evidence-based approaches designed to optimize each stage of the patient journey, preoperative, intraoperative, and postoperative, combining advanced analgesia, personalized anesthesia, early mobilization, and optimization of all care. Currently, studies report varying degrees of complication rates; however, with careful preoperative planning, stringent intraoperative controls, and streamlined workflows that reduce operative time, some experienced practitioners report complication rates (involving infection, dislocation, loosening, or venous thromboembolism) of under 1%. Rates of 2–3% are often considered typical in comparable cohorts.
Enhanced Recovery After Surgery (ERAS) Protocol
ERAS is a patient-centered, multimodal program aimed at reducing the physiological stress of surgery and expediting recovery. Key components include:
- Preoperative Optimization: Patient education, nutritional support, anemia correction, and cessation of smoking/alcohol use.
- Multimodal Analgesia: Combines various pain control strategies (e.g., regional anesthesia, NSAIDs, acetaminophen) to reduce opioid use and its side effects.
- Minimally Invasive Techniques: Techniques that reduce tissue trauma, blood loss, and hospital stay.
- Early Mobilization: Walking on the same day or the next morning helps prevent complications like blood clots and pneumonia.
- Fluid and Temperature Management: Precise control of intraoperative fluids and body temperature reduces surgical stress and speeds healing.
Rapid Recovery Protocol
Rapid Recovery Protocols are an extension of ERAS, specifically adapted for joint replacement. They emphasize:
- Standardized Care Pathways: Streamlined coordination among surgeons, anesthesiologists, nurses, and physiotherapists.
- Goal-Oriented Rehabilitation: Early initiation of physiotherapy focused on functional independence, such as standing, walking, and climbing stairs, often within hours of surgery.
- Shortened Hospital Stay: Some patients are discharged within 1-2 days or even the same day, depending on their condition and support at home.
Multimodal Therapy
Multimodal therapy combines several treatment methods to improve outcomes and reduce the risk of complications:
- Pain Management: A combination of pharmacologic and non-pharmacologic strategies (e.g., cryotherapy, nerve blocks) to control pain.
- Rehabilitation: Tailored physical therapy plans focus on promoting strength, flexibility, and gait training, with continued support transitioning into outpatient or home-based rehabilitation.
- Psychological Support: Mental preparedness and counseling can reduce anxiety and improve participation in recovery efforts.
Other Surgical Approaches in Hip Replacement
Posterior Approach
This technique for total hip replacement involves an incision near the buttocks, providing excellent visibility of the hip joint.
- Advantages: Offers a direct line of sight to the hip joint, facilitating precise implant placement. Typically linked to fewer complications than other approaches.
- Risks: Slightly higher risk of postoperative dislocation, particularly in the early recovery period. Specific movement precautions are often recommended to lower this risk.
- Recovery: Usually requires a moderate recovery period, with most patients resuming activities in a few months.
Anterior Approach
This approach accesses the hip joint from the front, avoiding the need to cut through major muscles.
- Advantages: The muscle-sparing technique potentially leads to quicker recovery and less postoperative pain. Some studies suggest lower rates of infection and dislocation compared to the posterior approach.
- Risks: Technically demanding and may have a steeper learning curve for surgeons. Potential for nerve injuries, such as lateral femoral cutaneous nerve (LFCN) damage, and higher rates of revision surgery in some cases.
- Recovery: Patients may experience a faster return to daily activities, but the risk of complications may be higher in certain populations.
Lateral (Anterolateral) Approach
The lateral approach uses a hip-side incision to access the joint through the muscles.
- Advantages: It provides good exposure to the hip joint and is associated with a lower risk of dislocation.
- Risks: Potential for muscle weakness, leading to a limp or gait abnormalities postoperatively. Longer rehabilitation may be required to restore muscle strength.
- Recovery: Recovery may be slightly longer compared to the posterior approach due to the need for muscle healing.
Common Reasons for Hip Replacement
Hip replacement surgery is typically considered when the joint has been significantly damaged by disease, injury, or structural abnormalities, and other treatments no longer provide relief. The following are the most common indications for total hip replacement (THR):
- Osteoarthritis - Degeneration of cartilage causes pain, stiffness, and limited mobility.
- Rheumatoid Arthritis & Inflammatory Conditions - Autoimmune inflammation damages joint cartilage and bone.
- Post-Traumatic Arthritis - Joint damage after hip injury leads to early arthritis.
- Hip Fractures or Trauma - Severe fractures (e.g., femoral neck, intertrochanteric, subtrochanteric) may require replacement.
- Avascular Necrosis - Loss of blood flow to the femoral head leads to bone death and collapse.
- Congenital/Developmental Hip Disorders - Abnormal hip development (e.g., DDH, Perthes) leads to early joint damage.
Less Frequent Indications
Rarely, primary bone tumors or metastatic cancer involving the hip may necessitate joint replacement as part of limb-sparing treatment. These cases require close coordination with oncologic specialists.
Symptoms Indicating a Need for Evaluation
You might be a candidate for hip replacement if you are experiencing:
- Persistent pain in the groin, thigh, or buttocks that does not improve with rest or medication. Unlike sciatica, which radiates down the leg, hip-related pain is often localized or deep in the joint.
- Interference with daily activities, such as walking, bending, dressing, or standing for prolonged periods.
- Sleep disturbances due to chronic pain and discomfort.
- Stiffness and reduced range of motion, often most noticeable in the morning or after long periods of inactivity.
- Limping or difficulty bearing weight, especially when transitioning from sitting to standing or using stairs.
These symptoms indicate joint degeneration that may warrant surgical evaluation, especially when conservative treatments such as physical therapy, injections, or medications no longer help.
What to Expect Before and During Surgery
Pre-surgery preparation may include blood tests, imaging, pausing medications, prehabilitation exercises, and lifestyle changes like weight loss or smoking cessation.
Typically done under general or spinal anesthesia, the procedure involves making an incision, removing damaged bone, placing the prosthesis, and closing the wound. The surgery typically takes 1-2 hours.
Risks and Potential Complications
Though generally safe, a few complications that may occur are listed below:
- Infection (e.g., periprosthetic joint infection).
- Blood clots in the leg or lungs.
- Dislocation of the new joint.
- Leg length discrepancy.
- Implant loosening or wear.
- Nerve or blood vessel injury.
- Fractures during or after surgery.
Long-Term Outlook
With proper care, most patients experience noticeable improvements in range of motion, pain relief, and quality of life.
Lifestyle Tips After Surgery
Maintaining a healthy weight is key to protecting joint health after surgery. Regular check-ups are also essential to monitor implant integrity and ensure long-term function. Recent advancements have enabled many individuals to resume low-impact exercises, such as cycling and swimming, as well as high-impact sports. However, while advanced recovery protocols and minimally invasive approaches have shown improved long-term prognosis, it is essential to follow your doctor's advice on any lifestyle or activity restrictions that might apply.
Long-Term Results
Studies show most patients maintain good function for 15–20 years after THR.
Alternatives to Hip Replacement
Though severe hip degeneration often requires surgery, non-surgical treatments may ease symptoms and may delay surgery.
- Biological Therapies
- Platelet-Rich Plasma (PRP) Therapy: Involves injecting concentrated platelets from the patient's own blood into the hip joint to promote healing and reduce inflammation. These therapies can also be used in conjunction with surgical procedures to enhance healing and improve outcomes.
- Bone Morphogenetic Proteins (BMPs): Proteins that stimulate bone growth and healing, potentially useful in certain surgical procedures.
- Stem Cell Therapy: Utilizes stem cells to regenerate damaged tissues, though its efficacy in hip joint repair is still under investigation.
- Medications: NSAIDs, corticosteroids.
- Lifestyle changes: Weight loss, avoiding impact activities to alleviate stress on the hip joint.
- Physical therapy: Targeted exercises for the muscles around the hip joint help improve stability and ease pain.
- Mobility aids: Canes or walkers.
- Injections: Cortisone or viscosupplementation.
Surgery becomes necessary when these interventions no longer provide relief, and quality of life is severely affected.
Conclusion
Hip replacement is often considered when significant joint damage persists despite conservative treatments. Although surgical innovations, updated recovery strategies, and personalized care before, during, and after the procedure have improved outcomes, deciding on surgery should follow a careful medical assessment that takes individual circumstances into account. In this regard, collaborating with an experienced healthcare professional helps support informed and personalized decisions. Through a combination of technology, innovative materials, and an individualized approach, hip replacement surgery can be transformative, enabling surgeons to achieve more predictable and satisfactory results with fewer complications and a noticeably improved quality of life for patients.

Dr. Inmaculada Gómez Arrayás is a specialist in orthopedic surgery and traumatology, with extensive experience in joint replacement surgery, having performed over 3,500 hip and knee prostheses. She heads the Traumatology and Orthopaedic Unit at Hospital Ruber Internacional from Quirónsalud Hospital Group. She is a pioneer in performing surgeries using navigation systems and rapid recovery techniques, and has been featured consecutively in Forbes magazine’s list of the 100 best doctors in Spain for several years.

Hospital Ruber Internacional, a part of the Quirónsalud Hospital Group, is a leading private hospital in Madrid, Spain, known for its top specialists, advanced technology, focus on innovation, and commitment to continual advancement in healthcare. The hospital offers cutting-edge treatments in various specialties, such as cancer, cardiovascular, and neurological conditions.
The Traumatology and Orthopedic Surgery Unit at Hospital Ruber Internacional combines advanced technologies, including robotic and navigation-guided systems, to enhance precision in hip and knee replacement surgeries. An adapted ERAS protocol supports faster recovery with fewer complications. The team also offers specialized microsurgery and regenerative therapies for complex injuries and preventive care. Backed by over 20 years of experience and ISO 9001:2008 certification, the center upholds a strong commitment to clinical excellence and patient safety.
References:
Featured Blogs



