PSORIASIS FACTS AND MYTHS

Article Updated 4 January 2024
Psoriasis is a chronic skin condition characterized by red patches with white, flaky skin prevalent on the elbows, knees, scalp, and legs. Psoriasis is not uncommon. According to the World Psoriasis Day Consortium, 125 million people worldwide or 2 to 3 percent of the total population have psoriasis.
Up to one-third of people with psoriasis may also have a form of arthritis called "psoriatic arthritis," in which the immune system also attacks the joints.
In many cases, psoriasis goes away and then flares up again. The triggers that bring on psoriasis include stress, dry air, infections, skin injuries, some medicines, too much or too little sun, cold weather, and smoking.
Psoriasis diagnosis is done by a dermatologist. The doctor may take a piece of the affected skin (a biopsy) and examine it under the microscope. When biopsied, psoriasis skin looks thicker and inflamed when compared to skin with eczema.
There are many misconceptions about Psoriasis. Here are some common myths people still believe about psoriasis.
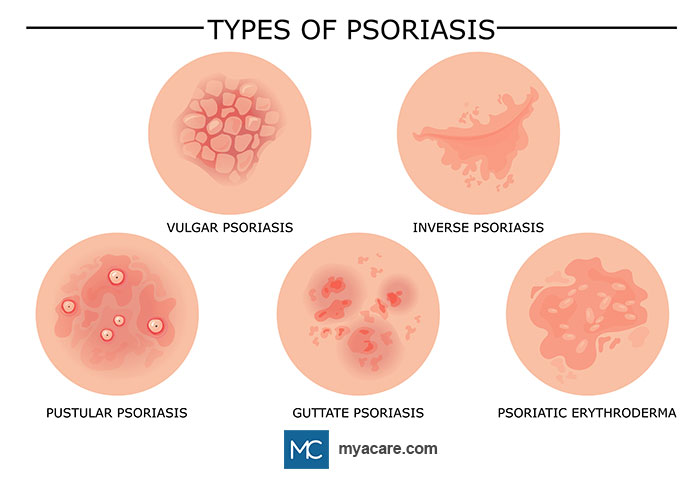
All Forms of Psoriasis Are the Same
As per the National Psoriasis Foundation, there are five different types of psoriasis:
- PLAQUE: It is one of the most common forms of Psoriasis identified by its layer of flaky dead skin cells called scales over raised red patches. It mainly affects the elbows, knees, scalp, and lower back but is not limited to these regions.
- GUTTATE: Unlike plaque psoriasis, guttate is characterized by red, scaly, tiny patches, often resembling spots, wherein spots cluster together on the skin. These spots, which show up mainly on the back, ears, or the scalp can develop into a mild and moderate lesion, covering between 3% - 10% of your body.
- PUSTULAR: As the name suggests, pustular psoriasis leads to the building up of white pustules or noninfectious blisters, which either appear in a small area like fingertips or spread across wider regions like palms or feet.
- ERYTHRODERMIC: It is the rarest form of psoriasis, affecting 3% of the total population, and is in the form of deep rashes characterized by severe pain and itching, fluctuating body temperature, and shedding of skin.
- INVERSE: Inverse or Hidden psoriasis, which it is commonly referred to as, affects those parts of the body where the skin rubs against skin or in the folds, such as arms and inner thighs. Another distinguishing characteristic of inverse psoriasis is that it appears as small patches, unlike any other form of psoriasis.
Only Adults Get Affected by Psoriasis
Psoriasis flares can start at any age. Up to 40% of people with psoriasis have symptoms before they are 16 years old, and 10% get it before they are 10. Although rare, infants can also get psoriasis.
If one of the parents has the disease, then there is a 10% chance that their child will develop it. If both parents contract psoriasis, then that child's rate of having psoriasis increases to 50%.
Psoriasis Is Contagious
Psoriasis skin can crack and bleed, leading people to believe that the infected skin is contagious, but Psoriasis is not contagious. Firstly, psoriasis is not an infection. It is an autoimmune disease wherein the immune system attacks itself.
In an autoimmune disease, the immune system develops cells, but considers them foreign cells and attacks them, leading to the disease. Autoimmune diseases like psoriasis are not transmitted from one person to another by any infectious element.
Bad Hygiene Causes Psoriasis
Psoriasis is inflammation deep within the epidermis and causes cracks and bleeding of the skin. It is caused by the immune system perceiving its cells as invaders and attacking them. It has nothing to do with cleanliness.
Psoriasis Cannot Be Managed
As mentioned above, psoriasis is a chronic autoimmune disease that cannot be cured. There is no treatment yet researched and found that can guarantee a complete cure for the illness.
However, there are treatments to help manage the condition. The most common form of treatment includes topical and internal medications that help to suppress the scaling and cracks. Organic treatment at home, such as oatmeal baths, yoga, and eating the right food can also help ease the itching and soothe the scales.
Phototherapy is being researched to provide an effective solution. In phototherapy, the part affected by psoriasis is exposed to natural or artificial light. Natural light is sunlight, and artificial light includes UVA or UVB. Overexposure to both natural and artificial light results in side effects.
Psoriasis Is Just Dry Skin
Contrary to popular belief, psoriasis is not simply dry skin. It is a chronic autoimmune disease that affects the skin cells, causing them to rapidly build up on the surface. This leads to the formation of thick, red, and scaly patches on the skin.
The underlying cause of psoriasis is deeper than the skin as well, and the condition typically leads to symptoms in other areas of the body.
Psoriasis Only Affects the Skin
Not only can psoriasis damage the skin, but it can also impact other parts of the body. While psoriasis is often characterized by red, scaly patches on the skin, it is actually a systemic disease that affects the entire body.
In psoriasis, an overactive immune system can result in symptoms that occur all over the body, such as joint pain, fatigue, and even an elevated risk of developing other health conditions like cardiovascular disease and diabetes.
Rare complications of psoriasis involving other body areas include:
- Psoriatic arthritis: As explained, systemic inflammation in psoriasis can lead to joint pain and damage due to an overactive immune system.
- Nail psoriasis: Psoriasis that affects the nails is known as nail psoriasis. Changes in the nails, including pitting, discoloration, thickness, brittleness, and detachment from the nail bed, may result from it.
- Uveitis: Psoriasis can sometimes cause uveitis, which is inflammation of the uvea, the middle layer of the eye. Uveitis can lead to redness, eye pain, blurred vision, and sensitivity to light.
Eczema and Psoriasis Are the Same
Although the difference might be difficult to explain, psoriasis is not the same as eczema. They are two distinct conditions with different causes and symptoms.
The causes of psoriasis are better understood than those of eczema. In psoriasis, the immune system causes the skin to grow too fast, leading to dead skin cell accumulation that resembles mildly itchy scales on the skin.
In eczema, the skin dries out a lot more and develops an intensely itchy rash. It’s unclear what causes eczema, although it’s suspected to be a combination of environmental, genetic, inflammatory, and/or autoimmune features.
Both conditions may respond to treatment with anti-inflammatories or topical steroids to suppress immune activity.
Patients with psoriasis typically respond to light therapy and get more sunlight[1], while those with eczema[2] do not. Those with eczema often need moisturizer more to ensure their skin is safe from infection.[3]
Psoriasis Affects Fertility
There is not enough evidence to support the notion that psoriasis directly affects fertility. There are a few preliminary studies that suggest a link between untreated moderate to severe psoriasis, reduced male and female fertility, and a higher degree of pregnancy loss.
It is important to consult with a healthcare professional for personalized advice, support, and adequate treatment.
Exercise Makes Psoriasis Worse
Exercise can actually have a positive impact on psoriasis. While intense exercise may cause temporary redness and flushing of the skin, regular physical activity can help manage stress, boost mood, and improve overall well-being.
It may also be a viable prevention measure for comorbidities that often present alongside psoriasis, such as heart disease, obesity, and mental health disorders. Obesity and related conditions can increase systemic inflammation and worsen the severity of psoriasis symptoms, while exercise can help combat weight gain and regulate immune activity.
It is important to choose activities that are comfortable and enjoyable and to take necessary precautions to protect the skin during exercise.
Facing the Facts About Psoriasis
While there are many misleading statements made about psoriasis, there are some astounding truths about the condition that are both insightful and hope-inspiring:
Genetics Increase the Risk of Developing Psoriasis
While having a family history of psoriasis does not guarantee that you will get the condition, it does increase the likelihood. Researchers have identified certain genes that are associated with psoriasis (namely CCHCR1, HLA-C, and CDSN), and having these genes can make a person more susceptible to developing the condition. It is believed that these genes influence the immune system and how it interacts with the skin cells, leading to an overactive immune response and the development of psoriasis.
However, it is important to note that genetics is just one factor. Not everyone with these genes will develop psoriasis, and not everyone without these genes will be free from the condition. Other factors, such as environmental triggers, also play a role in the development of psoriasis.
Watching Your Diet Might Help Lessen Psoriasis Severity
Although there is no special diet for psoriasis, there are dietary modifications that may help with symptoms.
Any food that triggers an allergic reaction or inflammation can possibly contribute towards flare-ups or worsening of symptoms. A person with psoriasis may benefit from cutting out highly processed foods and foods high in sugar or saturated fats. Keeping a food diary or using a diet tracking app can help those with the condition to identify possible trigger foods consumed near the time of a flare.
Some studies suggest that a well-balanced diet rich in fruits, vegetables, whole grains, and lean proteins may have a positive impact on psoriasis. These serve to lower inflammation and maintain a healthy weight. Some with psoriasis benefit from opting for a Mediterranean diet[4], a vegetarian diet, and/or a gluten-free diet.
Additionally, those with psoriasis may benefit from the following nutrients, which can be found in supplements and throughout a balanced diet plan:
- Vitamin A, C, E and D3
- Carotenoids and other antioxidant flavonoids (these can be found in a variety of brightly colored plant-based foods)
- Selenium
- Omega-3 fats and other poly-unsaturated fats
Stress and Strong Negative Emotions Can Trigger Psoriasis Flares
Stress is known to be a trigger for flare-ups in 31-88% of psoriasis patients. Many patients contract the disease after a majorly stressful event, and unfortunately, stressing over the condition itself often creates a vicious cycle of stress-induced flare-ups.
Strong emotions and high levels of stress can impact the immune system and potentially worsen psoriasis symptoms. Researchers are still figuring out why this is the case. The nervous response to stress appears to be altered in those with psoriasis, causing the brain to send out signals to the skin that mobilize the immune system to the area. The immune system may also respond to stress hormones like cortisol in a way that causes excess inflammation[5], leading to excessive dead skin accumulation and psoriasis scales.
Finding good coping mechanisms for stress is crucial, such as through exercise, relaxation techniques, or seeking support from healthcare professionals.
Talking and Being Social Can Improve Symptoms
Talking can help improve symptoms in those with psoriasis by providing emotional support and reducing stress levels. Psoriasis is a chronic illness that can seriously affect a person's mental and emotional health. It is not uncommon for individuals with psoriasis to experience feelings of embarrassment, self-consciousness, and frustration due to the visible symptoms of the condition. Talking to someone close can lessen these feelings, promote mental well-being, and reduce flare risk by helping lower stress.
Infections and Tonsillitis Can Make Psoriasis Worse
Infections, particularly streptococcal infections that cause tonsillitis, have been known to trigger or worsen psoriasis symptoms in some individuals. For those with chronic tonsilitis, having the tonsils removed (tonsillectomy) might be a viable treatment option that improves psoriasis symptoms.
It is important to maintain good overall health and seek medical treatment for any infections to help manage psoriasis.
Not All Home Remedies Are Ineffective
According to some sources, ice packs or cold water immersion[6], topical apple cider vinegar[7], and bathing the area (in water that is not too hot) can all help to soothe the itching.
As explained above, flavonoids, vitamins, and other antioxidants can help when part of the diet, yet they can also help soothe inflammation in the skin when applied topically.
Despite these, not all of them will work for everyone, and they should not replace advice or treatment from a certified dermatologist. If you have symptoms of psoriasis, it’s best to get treated as soon as possible.
Conclusion:
Psoriasis is a chronic autoimmune disease, but scientists and doctors across the world are diligently working to find the root cause of it and develop a medicine to help patients get relief from the physical and emotional pain.
Just like any disease, Psoriasis should not be stigmatized. There are many foundations helping psoriasis patients break out of the stigma. Educating people about psoriasis is part of a national and international patient care research process. Healthcare services throughout the world are trying to educate the public, patients, and guardians about the disease.
To search for the best health providers for dermatology in Croatia, Germany, Greece, Italy, Malaysia, Singapore, Slovakia Spain, Thailand, The UAE, the UK, and the US, please use our free search engine.
To search for the best doctors and healthcare providers worldwide, please use the Mya Care search engine.
References
- https://www.webmd.com/skin-problems-and-treatments/psoriasis/pediatric-psoriasis-facts#1
- https://www.psoriasis.org/about-psoriasis
- https://www.verywellhealth.com/psoriasis-is-not-contagious-4158175
- https://www.verywellhealth.com/psoriasis-an-autoimmune-condition-3876757
- https://www.livescience.com/32256-does-cold-weather-cause-colds.html
- https://www.psoriasis.org/about-psoriasis/types/erythrodermic
- https://www.webmd.com/skin-problems-and-treatments/psoriasis/plaque-psoriasis-facts#1
- https://www.webmd.com/skin-problems-and-treatments/psoriasis/guttate-psoriasis#1
- https://www.healthline.com/health/pustular-psoriasis#types
- https://www.healthline.com/health/erythrodermic-psoriasis#symptoms
- https://www.healthline.com/health/inverse-psoriasis
- https://www.mayoclinic.org/diseases-conditions/psoriasis/diagnosis-treatment/drc-20355845
- [1] https://rheumatology.org/patient-blog/psoriasis-and-the-sun-helpful-or-harmful
- [2] https://www.healthcentral.com/condition/eczema/sun-and-eczema
- [3]https://eczema.org/information-and-advice/triggers-for-eczema/sun-and-eczema/
- [4] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6143029/
- [5] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8705845/
- [6] https://www.medicalnewstoday.com/articles/how-to-relieve-psoriasis-itch#cold-compresses
- [7] https://www.psoriasis.com/psoriasis-patients/tips/home-remedies-for-psoriasis
Disclaimer: Please note that Mya Care does not provide medical advice, diagnosis, or treatment. The information provided is not intended to replace the care or advice of a qualified health care professional. The views expressed are personal views of the author and do not necessarily reflect the opinion of Mya Care. Always consult your doctor for all diagnoses, treatments, and cures for any diseases or conditions, as well as before changing your health care regimen. Do not reproduce, copy, reformat, publish, distribute, upload, post, transmit, transfer in any manner or sell any of the materials in this blog without prior written permission from myacare.com.