What Is Roemheld Syndrome?

Medically Reviewed and Updated by Dr. Sony Sherpa, (MBBS) - July 09, 2025
Between 1910 and 1920, Dr. Ludwig Roemheld studied the phenomenon in which patients suffering from digestive problems and no detectable heart issues would experience cardiac symptoms. By the 40's, his research received more attention, and the medical community would eventually accept the existence of a gastro-cardiac symptom complex, also known as the Roemheld Syndrome (RS). Gastrocardiac syndrome, another term for Roemheld Syndrome, underscores the connection between gastrointestinal disturbances and cardiac symptoms. The most common model known for Roemheld Syndrome involves some gastrointestinal problem or disease that leads to arrhythmia or other types of abnormal heart rate issues. Although the precise interactions involved in Roemheld Syndrome are not well-described, anatomical proximity, the vagus nerve (VN), and electrolyte deficiencies are still considered equally valid candidates for the key element in Roemheld Syndrome, with VN being a well-supported option.
Roemheld Syndrome is not a disease; it is just a particular combination of symptoms appearing together being caused by one or more pathologies. Although in the first publications discussing this phenomenon several authors (including Roemheld himself) mention how “frequent“ it was to see patients with gastrointestinal diseases presenting RS, very little information about this syndrome’s epidemiology is available today. In fact, observing Roemheld Syndrome, personally seems to be so rare that a big portion of all modern publications on this topic tend to be case studies about individual patients. Overall, even patients with the exact conditions to be diagnosed with Roemheld Syndrome, usually aren’t, the connection between the guts and heart symptoms is made, but the syndrome is rarely mentioned.
In this article, we will examine the available information for Roemheld Syndrome and provide hard facts about its causes, specific symptoms, people at risk, diagnosis, treatment, and prevention.
Causes
Since the 1920’s, it is well-known that the primary cause of Roemheld Syndrome, is the accumulation of gas in the gastrointestinal (GI) tract. Initially, physicians assumed that those who experienced RS were producing more gas than usual though fermentation (part of the normal processes of digestion), however, as time went on, it became clear that for a great majority of cases, the problem wasn’t the gas produced, but the gas ingested.
A phenomenon called aerophagia (the excessive swallowing of air) seemed to be more pronounced in individuals with Roemheld Syndrome. It’s considered that any condition that promotes aerophagia will also increase the risk for Roemheld Syndrome.
The gas is “the problem” that leads to RS, however, for someone to develop this condition, the vagus nerve is key. If this nerve can be easily overstimulated by the stress in the GI tract, then it is much more likely for the heart’s rate of pulsations per minute to become affected (normally decreasing to then increase rapidly). Considering this, a pre-existing or easily producible vagotonic condition could also be considered as a cause (or at least a main contributing factor) for Roemheld Syndrome.
What Causes Roemheld Syndrome Symptoms?
When Ludwig von Roemheld first described the syndrome, he observed that the symptoms were not rooted in cardiac issues but rather in the gastrointestinal tract. The primary cause of the symptoms was identified as the excessive accumulation of gas in the stomach and intestines.
Additionally, anatomical conditions, such as a hiatal hernia (where the stomach slides through the diaphragmatic opening towards the esophagus), also contribute to the development of symptoms associated with Roemheld syndrome.
The increased volume in the gastrointestinal tract results in the diaphragm being pushed towards the chest cavity. Under normal conditions, the diaphragm, located below the lungs, acts as a crucial respiratory muscle and serves as a partition between the chest and abdominal cavities.
When displaced into the chest cavity, the available space for the lungs and heart is reduced, leading to compression and a variety of symptoms. The heart's ability to beat regularly is compromised, causing typical cardiac symptoms. Similarly, the lungs cannot expand fully, resulting in breathing difficulties and shortness of breath.
- Heart problems arise because the pressure on the diaphragm constricts the heart within its chest cavity (mediastinum), preventing it from developing its full pumping power.
- Shortness of breath occurs due to the elevated position of the diaphragm, which exerts pressure on the lungs. This makes it difficult for the diaphragm to contract fully, resulting in breathing challenges.
- Hot flashes are a consequence of impaired cardiac function, which triggers the activation of the autonomic nervous system, specifically the sympathetic nervous system responsible for the "fight or flight" response. This activation can lead to the sensation of hot flashes.
- Anxiety is often triggered by the activation of the autonomic nervous system and the sensation of pain in the heart area, leading to acute anxiety episodes.
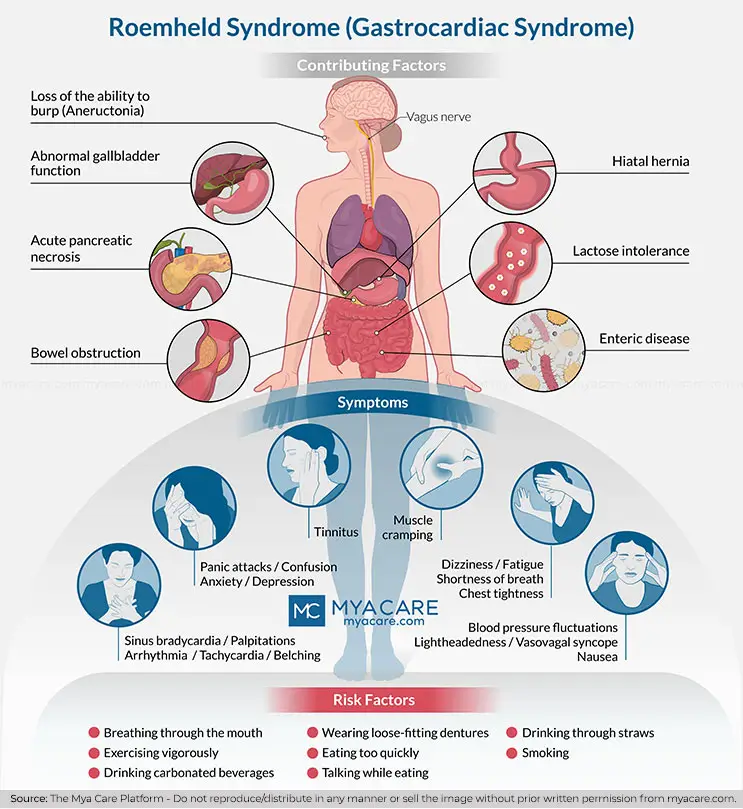
- Lactose intolerance
- Abnormal gallbladder function
- Hiatal hernia
- Enteric disease
- Loss of the ability to burp (Aneructonia)
- Bowel obstruction
- Acute pancreatic necrosis
Symptoms
- Sinus Bradycardia (slow heart rate)
- Shortness of Breath
- Chest tightness
- Muscle cramping
- Dizziness
- Palpitations
- Belching, nausea
- Arrhythmia (irregular heart beat)
- Tachycardia (rapid heart rate)
- Panic attacks
- Confusion
- Anxiety
- Depression
- Blood pressure fluctuations
- Lightheadedness
- Vasovagal syncope (fainting)
- Tinnitus (ringing in the ears)
- Fatigue
- Heartburn behind the breastbone
- Hot flashes
People at risk
As we mentioned before, aerophagia is an important element in Roemheld Syndrome, and those with this condition will be at a higher risk of developing the syndrome.
Aerophagia is common in people who have the habits of:
- Eating too quickly
- Talking while they eat
- Drinking through straws
- Smoking
- Breathing through their mouths
- Exercising vigorously
- Drinking carbonated beverages
- Wearing loose-fitting dentures
People with respiratory problems who use medical equipment to alleviate their condition are also at risk. Sleep apnea is a good example; usually, this condition requires the patient to use a Continuous Positive Airway Pressure Machine (CPAPM) in the form of a mask. If the air pressure being generated by the machine is not properly calibrated or there are some congestion problems, a lot of air will be swallowed. In general, any need for long-term assisted breathing will increase the risk of aerophagia and Roemheld Syndrome.
In the 1920’s, researchers also noticed that those of “nervous predisposition” were more likely to develop symptoms. By today's standards, this means that those struggling with anxiety are also at risk.
People with an overstimulated vagus nerve, such as those with vasotonic angina will have the right conditions to manifest the syndrome; however, very little is known about the precise vagotonic conditions that could be related to higher or lower risk. People with symphathicotonic conditions will also be vulnerable.
Pathologies that lead to weakness of the superior esophageal sphincter (like cricopharyngeal fibrosis) can also increase the risk for Roemheld Syndrome, since they allow more air to enter the GI tract. A good example of this is the link that seems to be between gastroesophageal reflux disease (GERD) and atrial fibrillation (AF). Up to 14% of people who suffer from GERD also experience AF.
Diagnosis
Diagnosing Roemheld Syndrome is not easy, and due to its nature, many will be misdiagnosed with either a non-existent heart condition or a mental issue. Patients’ experiences will vary considerably depending on which doctor they visit first.
Since the most obvious symptoms of Roemheld Syndrome are very similar to those belonging to many different cardiac diseases, most patients will visit a cardiologist first. Most doctors will focus on finding a heart problem that is not really there. With that purpose, they will use diagnostic tools like EKG’s, Holter monitors, slope tests, cardiac MRIs, cardiac CTs, cardiac catheterizations, EP studies, Echocardiograms, and many blood tests. Sleep studies may even be included. If everything goes well, no heart condition will be found.
Some patients are put under psychological examination to detect any signs of anxiety, depression, or a conversion disorder. Mainly because their symptoms will appear to have no physical cause.
Gastroenterologists have the best chance of diagnosing RS in symptomatic patients by performing colonoscopies, endoscopies, and ultrasounds. This way, a doctor will be able to detect the presence of a gastrointestinal problem (leading to a distended GI tract).
Linking the cardiac symptoms to the GI issues is more difficult. Roemheld Syndrome, diagnosis at this point is not an exact science and only recently the medical community has started to consider this type of association between the digestive and circulatory systems in the context of treating arrhythmias.
If Roemheld Syndrome is suspected by a doctor, a combination of X-rays and EKGs to detect simultaneous air-filled bowels and arrhythmia has been used for effective diagnosis; However, improvement of cardiac symptoms after treatment of the gastric conditions is the strongest confirmation for Roemheld Syndrome.
Treatment
- Anticholinergics or magnesium/ sodium supplements to raise blood pressure
- Anticonvulsants like Lorazepam and Oxcarbazepine help regulate motility in the GI tract and the vagus nerve
- Alpha and beta blockers to increase motility and regulate heart rate respectively
- Antigas to reduce gastric pressure. In this category, Simethicone is very popular
- Antacids help against acid reflux
Diet for Roemheld Syndrome
Managing Roemheld Syndrome involves addressing dietary habits to reduce the symptoms caused by gastrointestinal issues.
Foods to Avoid
- Carbonated Drinks: These can increase gas accumulation in the stomach and intestines, exacerbating symptoms.
- Fried and Fatty Foods: These are harder to digest and can slow down gastric emptying, leading to increased gas production.
- Certain Vegetables: Vegetables such as beans, cabbage, onions, and broccoli are known to cause gas and should be avoided.
Foods to Eat
- Easily Digestible Foods: For smoother digestion and less gas, opt for easily digestible foods like rice, bananas, and applesauce.
- Probiotics: Incorporating probiotics into the diet can improve gut health and reduce symptoms associated with Roemheld Syndrome. Fermented foods, such as yogurt and kefir, are powerhouses of probiotics.
Additional Dietary Tips
- Replace large meals with smaller, frequent meals - Overeating or consuming large portions can increase the pressure on the diaphragm and digestive system, leading to more pronounced symptoms. Smaller, frequent meals may help lessen this pressure and promote smoother digestion.
- Chewing Food Thoroughly: Ensuring that food is well-chewed before swallowing can aid digestion and reduce the amount of air swallowed.
- Avoiding Straws: Drinking directly from a glass instead of using straws can reduce the intake of excess air.
- Hydration: Staying well-hydrated with water can aid digestion and reduce gastrointestinal discomfort.
Prevention
A healthier lifestyle and reducing some of the behaviors that lead to gas accumulation in the intestines will help prevent RS.
- Eat slowly and with your mouth closed
- Don't smoke
- If you need assisted breathing, check with your doctor to determine if your equipment is properly calibrated.
- Follow a reduced FODMAP diet. It will help prevent gas accumulation
- Use magnesium supplements and regular exercise to make your heart stronger
Latest Research on Roemheld Syndrome Treatment
Recent advancements in the understanding and treatment of Roemheld Syndrome focus on several innovative approaches:
- LINX Magnetic Sphincter Augmentation: LINX magnetic sphincter augmentation is a minimally invasive surgery that involves strengthening the lower esophageal sphincter by implanting a ring of magnetic beads. This device helps to enhance sphincter function and prevent reflux. By reducing gastroesophageal reflux, the procedure can alleviate symptoms related to Roemheld Syndrome. LINX augmentation has been shown to significantly improve quality of life and reduce reflux symptoms in GERD patients.
- Fundoplication Surgery: Fundoplication is another surgical intervention aimed at treating GERD, which often coexists with Roemheld Syndrome. This surgery reinforces the sphincter between the esophagus and stomach by wrapping the upper stomach around the esophagus, preventing acid reflux. Fundoplication has been found to be effective in reducing symptoms of acid reflux and improving esophageal function, which can help alleviate the cardiac symptoms associated with Roemheld Syndrome.
- Vagus Nerve Stimulation (VNS): VNS is a treatment that involves stimulating the vagus nerve to manage symptoms. Excessive gas can overstimulate the vagus nerve, which regulates heart rate and digestion, potentially causing cardiac symptoms. VNS treatments aim to normalize nerve function and reduce the impact on the heart, offering promise in alleviating symptoms of Roemheld Syndrome.
FAQs
1. What are the long-term implications or potential complications of untreated Roemheld Syndrome?
Untreated or poorly managed Roemheld Syndrome may have potential long-term implications and complications. Chronic or recurrent episodes of excessive gas, bloating, and abdominal discomfort can lead to decreased quality of life and ongoing digestive issues. In some cases, persistent gas can contribute to esophageal or gastric reflux, potentially causing erosion or damage to the lining of the esophagus. Additionally, prolonged episodes of gas and bloating can result in malnutrition due to decreased appetite and poor nutrient absorption. Proper diagnosis and management are important to prevent these potential complications.
2. Is there ongoing research or emerging treatments for Roemheld Syndrome, and what advancements can be expected in the future?
It is worth noting that medical research is continually evolving, and new treatment approaches may be explored in the future. Gastroenterologists and researchers may investigate the efficacy of medications that can alleviate symptoms, such as antacids, prokinetics, or drugs targeting specific mechanisms of excessive gas production. Non-medication strategies, such as specialized diets or probiotic interventions, may also be areas of research interest. It is important to consult with healthcare providers to stay informed about the latest advancements in managing Roemheld Syndrome.
3. Can vigorous or intense exercise increase the risk of Roemheld syndrome?
Vigorous activities, such as weightlifting, can significantly increase intra-abdominal pressure, potentially leading to stomach compression. This, in turn, may push gastric contents upward into the esophagus, triggering acid reflux. Acid reflux is a recognized risk factor for arrhythmias, which are characteristic of Roemheld syndrome.
Intense exercise also causes rapid, forceful diaphragm contractions.
These movements can further contribute to the upward movement of stomach contents, potentially worsening reflux and causing symptoms like chest discomfort, heart palpitations, and shortness of breath.
4. Can Roemheld Syndrome cause a heart attack?
Roemheld syndrome may cause chest pain and palpitations that resemble a heart attack, but it does not actually cause one. It is essential to differentiate between cardiac issues and Roemheld syndrome. Severe symptoms warrant prompt medical attention to exclude potential heart-related problems.
5. Can stress/anxiety worsen Roemheld Syndrome symptoms?
Yes, stress and anxiety can exacerbate Roemheld syndrome symptoms. Stress can heighten vagus nerve sensitivity, which in turn may worsen gastrointestinal distress. Relaxation strategies, including deep breathing and mindfulness, are effective in managing stress-related symptoms.
6. Are there any tests specific to Roemheld Syndrome?
There is no single test for Roemheld syndrome. Diagnosis typically involves ruling out heart-related conditions and correlating gastrointestinal symptoms with cardiac-like symptoms. Tests may include electrocardiograms and clinical history review.
7. Can Roemheld syndrome be misdiagnosed as Anxiety Disorder?
Roemheld syndrome is sometimes misdiagnosed as an anxiety disorder because its symptoms, such as palpitations and chest discomfort, can overlap with those of anxiety. However, unlike anxiety, Roemheld syndrome is caused by gastrointestinal issues that affect the heart.
8. Can sleep apnea worsen Roemheld Syndrome?
Sleep apnea can exacerbate Roemheld syndrome. Frequent interruptions in breathing during sleep can increase intra-abdominal pressure, leading to worsened symptoms of reflux and arrhythmias.
9. Is Roemheld syndrome fatal?
Roemheld syndrome is not typically fatal, but if left unmanaged, it may lead to serious complications such as severe arrhythmias that can become life-threatening. Proper care and treatment play a key role in reducing these complications.
To search for the Best Gastroenterologists and Cardiologists in India, London, Thailand and Malaysia, please use the Mya Care search engine.
The Mya Care Editorial Team comprises medical doctors and qualified professionals with a background in healthcare, dedicated to delivering trustworthy, evidence-based health content.
Our team draws on authoritative sources, including systematic reviews published in top-tier medical journals, the latest academic and professional books by renowned experts, and official guidelines from authoritative global health organizations. This rigorous process ensures every article reflects current medical standards and is regularly updated to include the latest healthcare insights.

Dr. Sony Sherpa completed her MBBS at Guangzhou Medical University, China. She is a resident doctor, researcher, and medical writer who believes in the importance of accessible, quality healthcare for everyone. Her work in the healthcare field is focused on improving the well-being of individuals and communities, ensuring they receive the necessary care and support for a healthy and fulfilling life.
References:
Featured Blogs



