Biological Treatments in Orthopedics: Solutions From Within

Musculoskeletal injuries to the bones, tendons, cartilage, and muscles can lead to long-lasting and debilitating pain. One of the most prevalent medical conditions, musculoskeletal pain, affects around 47% of the general population.
Orthopedic treatment of musculoskeletal injuries, such as fractures, normally focuses on reconstructive approaches to anatomy and joint function. However, regenerative orthopedics is an innovative approach to wound healing and tissue regeneration. It utilizes the body’s biological substances, such as growth factors and stem cells, to promote wound repair and speed recovery.
What Is Regenerative Orthopedics?
Regenerative orthopedics is a novel field in restorative medicine that focuses on healing injuries and repairing damaged tissues using biological substances (also referred to as orthobiologics) from the patient’s own body.
So what is Orthobiologics? These are biological substances, or simply biologics, including growth factors, autologous blood products (platelet-rich plasma or PRP), and stem cells. These regenerative biologics are injected into the injured area of the body to promote healing and tissue regeneration.
In orthopedics, biological therapy can help treat musculoskeletal conditions and injuries, such as bone fractures, anterior cruciate ligament (ACL) tears in the knee, and sprained ankles.
Why Use Biologics In Orthopedics?
Regenerative biologics used in orthopedics aim to improve clinical outcomes when treating orthopedic injuries.
Tissues in the body heal naturally through biological processes. However, orthopedic medicine often omits the role of biologics in the healing process.
Naturally, the body uses its cells and growth factors to repair tissues and heal injuries. Orthobiologic injections speed up and boost the body's natural healing process by providing the building blocks for tissue repair.
So how do biologics work? Essentially, orthobiologics work by enhancing the body’s healing responses and tissue regeneration.
The latest treatments in regenerative medicine and biologics aim to achieve the following:
- Restore the anatomy of the injured or damaged area in the body
- Recover the function of the knee, ankle, shoulder, or another injured area
- Avoid or delay surgical interventions
The Role Of Growth Factors In Wound Healing
Growth factors have several roles that make them good candidates to be used as biologics in regenerative therapy. Growth factors are cytokines; small signaling proteins that control the growth and activity of other cells. They can regulate key events in tissue repair.
Growth factors, such as TGFB1, PDGF, and IGF-1, have the following integral functions in wound healing:
- They attract healing cells into the wound
- They stimulate the proliferation of these cells
- They affect the synthesis of the extracellular matrix, which is essential for tissue repair
Other growth factors, such as VEGF, HGF, and bFGF, can attract and stimulate the growth of endothelial cells, facilitating the formation of new blood vessels.
Thus, growth factors promote angiogenesis and vascularization, which is essential for wound healing. Angiogenesis is the growth of blood vessels from an existing vascular network. On the other hand, vascularization involves the formation of blood vessels and capillaries within a living tissue to improve oxygen and nutrient supply.
How Can We Use Growth Factors To Promote Wound Healing?
All types of connective tissue, including bone, cartilage, muscle, tendons, ligaments, and skin, contain many growth factors that play an integral role in remodeling and repairing damaged tissue.
Plasma drawn from the blood contains a high concentration of platelets. Platelets can carry proteins, including growth factors, to the injury site and improve healing. Therefore, we use platelets as vehicles to deliver those growth factors to the injured area.
In regenerative orthopedics, we deliver plasma-rich growth factors (PRGF) to the injury, where they can mimic the physiologic process of tissue repair. PRGF is a subtype of PRP derived from the patient's blood and tissue by separating whole blood into its components. PRGF stimulates tissue healing and bone regeneration.
The latest advanced nonsurgical and regenerative treatments of ligament, muscle, and tendon injuries include PRGF - Endoret.
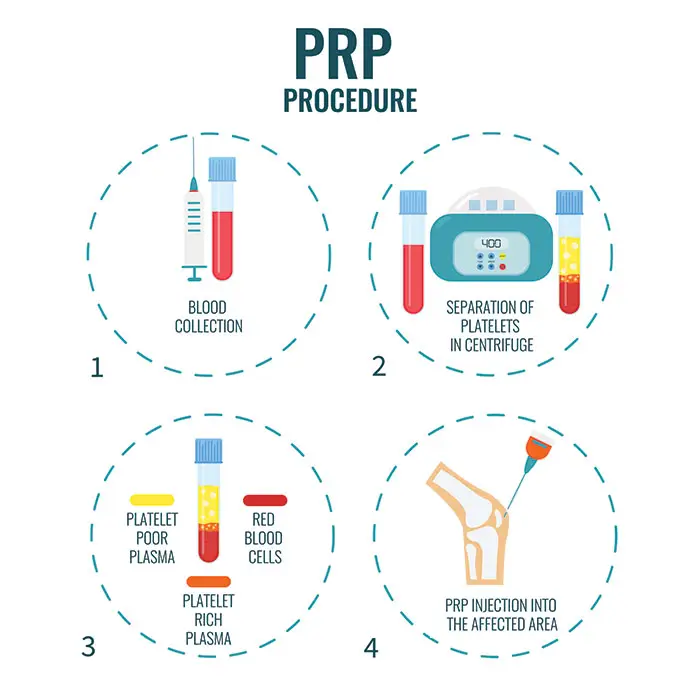
PRGF – Endoret: This plasma-rich in growth factors technique involves drawing a small amount of the patient’s blood, separating the platelets, then reinjecting them at the area of injury to aid tissue healing and regeneration.
Endoret - PRGF has the following characteristics:
- It contains plasma and platelets
- It is free from leukocytes, red blood cells, and inflammatory proteins
- It has 2 to 2.5 times the number of platelets found in venous blood
- It is easily activated with calcium dichloride (Cl2Ca)
Preparation of Endoret - PRGF from a patient’s blood involves the following steps:
- The patient’s blood is drawn
- The blood is centrifuged to separate its components
- The plasma-rich growth factors are activated
- The PRGF injection is administered at the area of the injury to speed up the healing
- It requires the patient to avoid food intake at least 4 hours before the blood extraction
The Role Of Stem Cells In Wound Healing
Stem cells are undifferentiated or partially differentiated cells. They have the unique ability to divide to form more stem cells or transform into various types of other body cells.
Stem cells can be obtained from the bone marrow (bone marrow concentrate) or fatty tissue (adipose-derived regenerative cells). The cells are then injected into the injured joint, tendon, or muscle to regenerate damaged tissue, stimulate growth factors, and improve wound repair.
These stem cells have become beneficial in orthobiologics and regenerative medicine because:
- They are easy to isolate
- They can divide and produce more stem cells
- They can differentiate into other types of cells, including cartilage, muscles, and bones
- They have powerful anti-inflammatory properties
- They can localize damaged tissue
Stem cell treatment is performed during orthopedic surgery and requires specific surgical skills and extensive background knowledge.
Adipose-derived regenerative cell (ADRC) therapy
Adipose-derived regenerative cell (ADRCs) therapy is another novel therapeutic approach in wound repair.
In this cell based therapy, an innovative technology called Lipogems harvests fat tissue rich in stem cells (adipose-derived regenerative cells). These adipose stem cells can be used to promote knee cartilage regeneration during ACL reconstruction surgery.
ADRCs can enhance wound healing by:
- Promoting new blood vessel formation
- Promoting matrix deposition and wound remodeling
- Preventing cell death
- Modulating inflammation
One study assessed the safety of incorporating stem cell therapy for knees by injecting Adipose-Derived Regenerative Cells (ADRCs) during the ACL reconstruction surgery of 20 football players. Patients receiving ADRC during their ACL reconstruction surgery had significant improvement in knee function and graft healing 12 months after the surgery.
Bone marrow concentrate (BMC)
The bone marrow is the part of the body where blood is produced. Stem cells taken from the bone marrow (bone marrow concentrate) by aspiration are specialized cells that can differentiate into various tissues and help speed up recovery.
BMCs can be used in chondral defect surgeries, i.e., to repair damage to the cartilage that lines the end of the bones.
BMC therapy can:
- Improve wound healing
- Improve tendon healing
- Enhance cartilage regeneration
- Improve bone consolidation in fracture treatment.
A study was conducted between 2013 and 2018 involving 278 football players with chondral injuries treated with BMC stem cell therapy for the knees during surgery for chondral defects. All the players had improved recovery and knee movement without any adverse effects three months after chondral surgery with BMC treatment.
Summary
Regenerative orthobiologics offer patients with musculoskeletal injuries novel treatments that can help them avoid long-term pain meds and sometimes even surgery.
Patients suffering from degenerative joint diseases or orthopedic injuries can receive some of the latest technologies in regenerative orthopedic treatments at leading specialized centers.

Dr. Ramon Cugat is a world-renowned leader in orthopedic surgery with ample experience and skills in complex techniques. As the director of the Instituto Cugat, at the Orthopedic Surgery and Traumatology Department at Hospital Quirónsalud Barcelona, and together with the innovation led by the Fundación García Cugat, he has pioneered the use of growth factors in regenerative orthopedics and sports medicine. Throughout his career, he has treated world-renowned athletes who have been able to return to their respective teams thanks to his medical expertise. As the founding member of the Spanish Arthroscopy Association, he specializes in orthopedic surgery and novel techniques in the orthobiologic treatment of knees, ankles, hips, and joints.

The Hospital Quirónsalud Barcelona, Spain, is at the forefront of utilizing advanced orthobiologic therapies as a part of regenerative orthopedics and sports medicine. The Orthopedic Surgery and Traumatology Department’s core values are to deliver high-quality care and research-based advances. All conditions of the locomotor system are addressed by professionals in sub-specialty divisions for the hand, shoulder, foot, orthopedic oncology, pediatric orthopedics, keyhole surgery, hip and knee replacement, and sports medicine. Patients stand to benefit from the latest therapies, advanced medical equipment, and compassionate care, with an emphasis on doctor-patient interaction.
Sources:
Featured Blogs



