Effective Patellar Tendinopathy Treatment: The Basas Spanish Squat and More

The Significance of Physical Therapy
Conventional Patellar Tendinopathy Treatments
Advances in Physical Therapy and Rehab
Patellar tendinopathy, commonly known as "jumper's knee" or tendonitis, is an injury involving the patellar tendon (the connector between the kneecap and the shinbone) that can lead to pain and inflammation. It is particularly prevalent among athletes and people engaged in sports or activities that involve a lot of jumping and knee extension, such as basketball, volleyball, and track and field events.
The terms patellar tendinopathy, patellar tendonitis (alternatively, patellar tendinitis), and patellar tendinosis are often used interchangeably. However, "tendonitis" implies inflammation of the tendon, while "tendinosis" refers to degeneration without inflammation. "Tendinopathy" encompasses both tendon inflammation and degeneration.
The impact of patellar tendinopathy can be significant, leading to pain, swelling, and reduced mobility, limiting performance and quality of life. Proper diagnosis and targeted treatment strategies are important to manage symptoms and facilitate recovery. Physiotherapy and exercises are often involved in first-line treatment and rehabilitation, with other options considered in more serious cases.
The Significance of Physical Therapy in Patellar Tendinopathy Management
Understanding Patellar Tendinopathy
The patellar tendon plays a pivotal part in knee movement, connecting the base of the patella (kneecap) to the tibial tuberosity, the bony bump on the front of the shinbone (tibia).
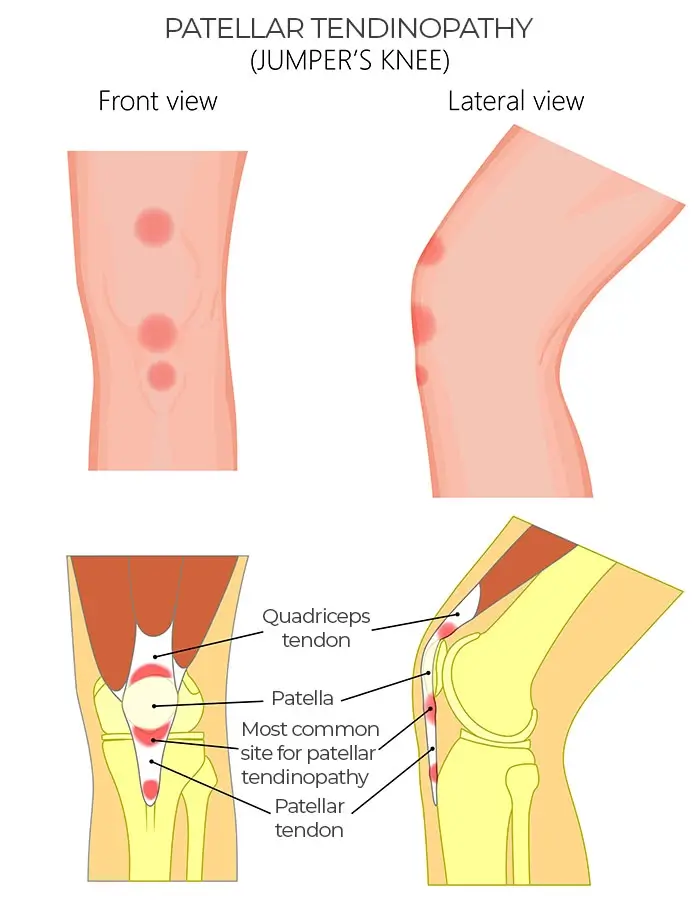
This tendon is a key component of the extensor mechanism of the knee, working alongside the quadriceps muscle and the quadriceps tendon to enable knee extension (straightening of the leg) and facilitate activities such as jumping, running, and walking.
Patellar tendinopathy can manifest in various types, traditionally categorized into tendinitis, tendinosis, and tears based on severity.
Chronic patellar tendinopathy is when the condition persists for several months or longer, often due to inadequate treatment or ongoing stress on the tendon. This stage is more challenging to treat and may require more complex interventions.
Common symptoms of patellar tendinopathy include:
- Anterior knee pain below the kneecap (at the base of the patella)
- Swelling and tenderness
- Weakness in the knee
- Pain that exacerbates during activities that involve knee extension, such as squatting and running.
- Difficulty performing activities that involve jumping or rapid changes of direction.
While treatment plans can vary case by case, physical therapy typically serves as a mainstay. Studies show that physical therapy can effectively address the underlying biomechanical issues and promote long-term benefits while enabling a personalized approach to minimize risk and recurrence.
Diagnosis
Diagnosing patellar tendinopathy involves a combination of clinical evaluation and imaging studies to identify the condition. Diagnosis typically starts with a doctor's review and physical exam. Specific tests, such as the "single-leg decline squat test," may be done to assess the tendon under stress.
To determine the degree of tendon damage and confirm the diagnosis, imaging tests like magnetic resonance imaging (MRI) and ultrasound are crucial.
Differential diagnosis is essential in the diagnostic process to distinguish patellar tendinopathy from other conditions that can mimic its symptoms. These include:
- Infrapatellar Bursitis
- Fat Pad Impingement
- Patellofemoral Pain Syndrome (PFPS)
- Plica Syndrome
- Osgood-Schlatter Syndrome
- Sinding-Larsen-Johansson Syndrome
Distinguishing "Jumper's Knee" vs. "Runner's Knee" is also crucial. While "Jumper's Knee" refers specifically to patellar tendinopathy, focusing on the patellar tendon's overuse and injury, "Runner's Knee" (PFPS) involves pain around the kneecap, often related to the patellofemoral joint and not necessarily linked to the patellar tendon.
Conventional Patellar Tendinopathy Treatment Options
Conventional treatment options for patellar tendinopathy aim to alleviate pain, reduce inflammation, and facilitate tendon healing. Among the initial treatment approaches is the RICE protocol, an acronym for Rest, Ice, Compression, and Elevation, which can be effective in managing acute symptoms. However, its limitations lie in addressing the root causes of tendinopathy, particularly in cases of chronic or degenerative conditions. It provides symptomatic relief but does not necessarily promote tendon healing or address biomechanical issues contributing to the condition.
Potential Downsides of Conventional Treatments
- Over-reliance on rest without appropriate physical therapy can lead to muscle weakness and stiffness.
- Prolonged use of ice and NSAIDs may mask symptoms, allowing people to return to activities prematurely and potentially exacerbate the condition.
- Compression and elevation are more effective for acute injuries and may have limited benefits for chronic tendinopathy.
- Surgery for patella tendon repair might be advised if physical and drug-based therapies prove unsuccessful. However, invasive procedures carry risks such as infection, nerve damage, and prolonged recovery times. There is also no guarantee of returning to pre-injury levels of activity.
Advancements in Physical Therapy and Rehab for Patellar Tendinopathy
Physical therapy and rehabilitation play a vital role in the treatment of patellar tendinopathy, addressing both symptom relief and the underlying causes of the condition. Physical therapy approaches typically include a combination of stretching, strengthening exercises, and massage aimed at improving flexibility, muscle strength, and tendon health.
The Basas Spanish Squat
The Basas Spanish Squat exercise is specifically designed to target the patellar tendon, enhancing strength and flexibility while minimizing stress on the knee. The unique feature of the Basas Spanish Squat is its ability to isolate and strengthen the muscles supporting the knee, applying a controlled load to the patellar tendon.
The exercise is based on biomechanical principles that ensure the knees do not extend beyond the toes, reducing shear forces on the patellar tendon. It encourages a posterior weight shift, engaging the glutes and hamstrings, thereby reducing the load on the patellar tendon.
Basas Spanish squat benefits include improved strength, flexibility, and reduced pain in people with patellar tendinopathy. When combined with electrical stimulation (E-stim), as indicated in some studies, it may enhance pain reduction and muscle activation, further aiding in the rehabilitation process. Electrical stimulation may help the tendon heal in ways that regular exercise alone cannot. As knee injuries often lead to weakened quadriceps muscles, E-stim can be especially beneficial in such cases as it forces muscle contractions to provide mechanical strain, even when voluntary control is limited. Furthermore, people with patellar tendon injuries sometimes subconsciously shift their body weight during exercise, reducing the targeted muscle's workload. E-stim helps overcome this by directly stimulating the muscle, ensuring it receives the necessary load for healing.
Finding the right balance of stimulation and repetition to maximize strain on the tendon while minimizing discomfort is crucial to using this technique effectively. Clinicians will tailor therapy in line with recommended guidelines based on existing research to each individual's needs for maximum comfort and benefit. This can involve measuring the strain on the tendon or the strength of the leg extension to help optimize the exercise program. Advanced imaging techniques can further confirm the effectiveness of this method.


Source: Quirónsalud Hospital Group
Other Effective Physical Therapy and Rehabilitative Treatment Approaches:
- Heavy Slow Resistance Training (HSRT) and Eccentric Loading Exercises: Focus on slow, controlled movements that support patellar tendon strengthening.
- Tendon Neuroplastic Training: Aims to retrain the brain's perception of pain and improve tendon function.
- Plyometrics and Neuromuscular Training: Gradual progression in these exercises can enhance the strength, function, and dynamic stability of the knee.
Manual Therapy
Advanced techniques such as dry needling, IASTM, and fascial manipulation can be used for targeted pain relief and to mobilize soft tissues, enhancing recovery.
Other Forms of Therapy
Emerging technologies such as Extracorporeal Shockwave Therapy (ESWT), laser therapy, and electrical stimulation are gaining attention for their potential benefits in managing patellar tendinopathy. ESWT delivers shockwaves to the affected area, stimulating blood flow and accelerating tissue healing.
Laser therapy utilizes light energy to reduce inflammation and promote tissue regeneration. Electrical stimulation can enhance muscle activation and decrease pain in the patellar tendon. However, these therapies should be part of a comprehensive treatment plan since their efficacy might vary, and research is still ongoing to fully understand their benefits and limitations.
Ultrasound-guided galvanic electrolysis is a minimally invasive technique that applies a galvanic current through a needle, targeting specific tissues to stimulate a healing response. While promising, its use requires further validation through clinical research.
Early findings on Blood Flow Restriction (BFR) therapy indicate potential benefits in reducing pain and improving function in those with patellar tendinopathy. It utilizes a cuff to restrict blood flow during exercise, allowing lighter weights to stimulate muscle growth with reduced tendon stress. This has shown promise in strengthening the muscles supporting the patellar tendon.
Personalized Rehabilitation Programs
Personalized rehabilitation programs are an innovative approach to treating patellar tendinopathy that leverages advanced diagnostic and monitoring technologies. By conducting detailed biomechanical assessments, therapists gain a comprehensive understanding of a patient's unique physical condition, including joint movements, muscle function, and overall body mechanics.
Gait analysis further adds depth to this understanding by evaluating the efficiency and patterns of movement as individuals walk or run, identifying any irregularities that may contribute to their condition or hinder recovery.
Electromyography (EMG) biofeedback is another critical component, offering real-time data on muscle activity. This information allows therapists to pinpoint areas of weakness or imbalance, facilitating the design of highly customized rehabilitation plans that address specific needs.
Such personalized programs are not static; they evolve based on continuous monitoring of the patient's progress. This dynamic approach ensures that the rehabilitation plan remains aligned with the recovery journey, allowing for adjustments as needed to optimize outcomes.
Recovery and Prevention
Successful recovery hinges on a gradual progression back to full activity, emphasizing the importance of listening to your body and not rushing the healing process. Managing pain with ice, rest, and appropriate physical therapy exercises is crucial during recovery. Preventing future occurrences of patellar tendinopathy involves regular stretching, proper warm-up and cool-down routines, and addressing any biomechanical issues with professional guidance. Proper footwear and the use of kinesio tape can also help prevent recurrences.
Expected Recovery Timeline
The recovery timeline for patellar tendinopathy can vary depending on the severity of the condition and the treatment approach. With proper treatment, patients may see improvement within weeks to months, but it is crucial to adhere to a tailored rehabilitation program to avoid setbacks.
Conclusion
Patellar tendinopathy is a condition that requires a multifaceted treatment approach to manage pain effectively, promote tissue healing, and prevent recurrence. The Basas Spanish Squat, particularly when combined with electrical stimulation, emerges as a valuable tool in a comprehensive physical therapy regimen.
Advances in physical therapy, along with emerging therapies like ESWT, laser therapy, and ultrasound-guided galvanic electrolysis, offer promising options for people suffering from patellar tendinopathy. However, the cornerstone of successful management remains early diagnosis, personalized treatment plans, and adherence to prevention strategies. As research continues to evolve, future therapies may offer even greater hope for those affected by this challenging condition.

Dr. Fernando Reyes heads the Physiotherapy and Rehabilitation unit at Olympia Sports Medicine Center. With over 25 years of experience working with esteemed organizations such as the Royal Spanish Basketball Federation, the Spanish Baseball Team, and Real Madrid CF, he has established himself as a trusted expert in his field. Dr. Reyes is a sought-after collaborator, providing rehabilitation and readaptation services to elite athletes at both national and international levels. His primary goal is to bring the same level of care and resources typically reserved for high-level athletes to the general athlete at Olympia. Through a multidisciplinary approach and a deep respect for biological processes, he aims to optimize recovery and provide athletes with the tools they need to achieve optimal performance.

Olympia, a part of Quirónsalud Group, is a one-of-a-kind healthcare project in Spain encompassing Sports, Lifestyle, and Medicine. The center comprises multidisciplinary medical units in sports, clinical and aesthetic nutrition, sleep medicine, high-performance psychology, cryotherapy, and many more. Featuring next-generation technological equipment and a team of renowned professionals, Olympia emphasizes innovation, knowledge, perseverance, and excellence to achieve sustainable, patient-centered health.
For more details, please visit https://olympia.quironsalud.com/
References:
Featured Blogs



