Fluorescence-Guided (FGS) Brain Tumor Surgery

Fluorescence-guided surgery (FGS) has recently been adapted to brain tumor surgery, and it promises to improve survival in patients being treated for brain cancer.
When it comes to brain cancer, surgery plays a key role in determining survival. The fewer cancer tissue is left after resection, the better the outcomes. Ultimately, the goal is to remove the tumor completely without leaving any malignant cells behind.
Unfortunately, this is not always possible. Many times, cancer cells seep into the surrounding brain tissue and cannot be differentiated from normal brain tissue.
Fluorescence-Guided Surgery (FGS) tackles this problem specifically. The use of fluorescent material makes the cancer cells glow, which guides the surgeon to perform better resection of the tumor.
Keep reading to learn more about brain cancer and how it’s being treated with Fluorescence-Guided Surgery (FGS).
What is a Brain Tumor?
A brain tumor is an abnormal growth that occurs in the brain. It can be either benign or malignant (cancerous). Malignant brain tumors are referred to as “brain cancer”.
As opposed to benign brain tumors, brain cancer has a malignant course and usually a bad prognosis.
Compared to other types of cancer, brain cancer is relatively rare. The chances of a person getting brain cancer during their lifetime are estimated to be around 0.6%.
Here are some key statistics related to brain tumors:
- Around 70% of brain tumors are benign, and 30% are malignant
- With benign tumors, the 5-year survival rate is on average 92%
- With malignant tumors (cancer), the 5-year survival rate is on average 36%
How serious brain cancer is and how long a person lives after the diagnosis depends on many factors. The age of the patient, type of brain tumor, and success of surgery are the most important factors in determining the prognosis.
What are the Types of Brain Tumors?
There are more than 150 reported types of brain tumors, and each is named after the type of cells that form it and its location.
Some tumors might have more than one name that refers to them (glioblastoma = type 4 astrocytoma).
Brain tumors are classified into malignant (cancer) and benign tumors:
- Benign: The most common of these is called meningioma. Other less-common types include pituitary adenoma, chordoma, craniopharyngioma, and others. These tumors are usually not deadly and can be completely cured with surgery alone.
- Malignant: Glioblastoma multiforme (GBM or Type 4 Astrocytoma) is the most common and most invasive type of malignant brain cancer. It usually has a bad prognosis with a median survival of 8 months. Other less common and less-invasive types include other gliomas, astrocytoma, medulloblastoma, and others.
Malignant tumors are further classified according to the severity of their type. Grade I and II tumors are low-grade tumors, while grades III and IV are considered high-grade tumors. For example, glioblastoma multiforme is classified as a Grade IV (high-grade) tumor.
This might get too confusing for some patients, however, doctors use these terms to guide treatment choices in patients and predict survival.
What is Fluorescence-Guided Surgery (FGS)?
Surgery is critical for the treatment of malignant brain tumors. A craniotomy (skull surgery) and tumor resection aim to remove as much of the tumor as possible. Ultimately, the goal is to leave zero malignant cells behind.
The challenge, however, is that invasive tumors, specifically glioblastoma multiforme, tend to “splash” themselves within the surrounding brain tissue. The malignant cells seep into the brain and between the normal cells in a thread-like fashion. This makes it extremely hard to tell them apart from normal brain cells when performing surgery.
To solve this problem, neurosurgeons have recently integrated a new technique for brain cancer surgery called Fluorescence-Guided Surgery.
This surgery uses “fluorophores” to make the tumor glow in a different color than normal tissue, making it easier for the surgeon to spot cancer cells.
Fluorophores include:
- Indocyanine Green (ICG)
- Fluorescein Sodium
- 5-Aminolevulinic ACID (5-ALA)
- Targeted Fluorophores
All of these are still being tested with different types of brain cancer to see which ones provide the best results. Fluorophores tend to accumulate in brain tissue for one or more of 3 reasons:
- Brain tumors have much more blood supply compared to normal tissue
- Some fluorophores tend to accumulate at areas with a disrupted blood-brain barrier
- Some fluorophores are combined with molecules that target tumor cells specifically
This increased tendency to accumulate in the tumor makes it possible to better visualize the extension of cancer during surgery.
How does Fluorescence-Guided Surgery for Brain Cancer Work?
Here’s the concept behind Fluorescence-Guided Surgery (FGS):
- The patient ingests or is injected with fluorophores before or during surgery
- Fluorophores will accumulate heavily in the brain tumor, but not in normal tissue
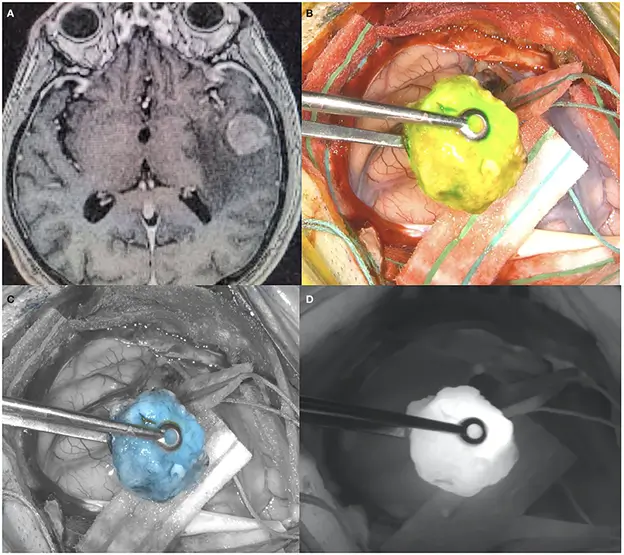
- During surgery, the neurosurgeon will use a special microscope lens to see the glow of the fluorophores (see image)
- The surgeon will resect all the tissue that’s glowing, leaving nothing behind
Despite enhancing the surgeon’s ability to resect more of the tumor, this does not mean that no cancer cells will be left behind. It does not mean that a full-cure is achievable.
Sadly, It is nearly impossible to remove all cancer cells with the current technology we have. Nevertheless, the more cancer is removed, the longer the survival. And that’s the benefit of Fluorescence-Guided Brain Surgery.
Which Cancers are Treated Fluorescence-Guided Surgery (FGS)?
Fluorescence-Guided Surgery has shown promise in helping treat several types of brain tumors, including:
- High-Grade Gliomas (Glioblastoma multiforme and others)
- Meningiomas
- Brain metastasis (extension of cancer from another body part, e.g. lung cancer)
- Pediatric Brain Tumors
- Spinal Cord Tumors
Is Fluorescence-guided surgery (FGS) Effective?
Fluorescence-Guided Surgery is a new and innovative surgical treatment for glioma, glioblastoma, and other brain cancer types.
It increases the accuracy and effectiveness of brain cancer surgery to make it more successful. This translates to better outcomes. In glioblastoma patients, for example, patients who received fluorescence-guided surgery:
- survived longer than those who received regular surgery (27 months vs. 17.5 months)
- had a higher rate of 6-month progression-free survival compared to those who received traditional surgery
- had a more complete resection of their tumor
This shows that fluorescence-guided surgery can extend the survival of patients with glioblastoma, and possibly delay the progression of their disease.
Outlook
Brain cancer is a serious diagnosis that still constitutes a big challenge for doctors.
Although fluorescence-guided brain surgery does not promise a full cure of brain cancer, it does give patients more precious time to spend with their loved ones.
In all cases, fluorescence-guided brain cancer surgery is a big step towards developing even better future techniques to hopefully cure brain cancer.
To search for the best Neurology Healthcare Providers in Croatia, Germany, India, Malaysia, Spain, Thailand, Turkey, Ukraine, the UAE, UK and the USA, please use the Mya Care search engine.
Dr. Mersad is a medical doctor, author, and editor based in Germany. He has managed to publish several research papers early in his career. He is passionate about spreading medical knowledge. Thus, he spends a big portion of his time writing educational articles for everyone to learn.
Sources:
Featured Blogs



