Insomnia in Older Adults: Causes and Treatment
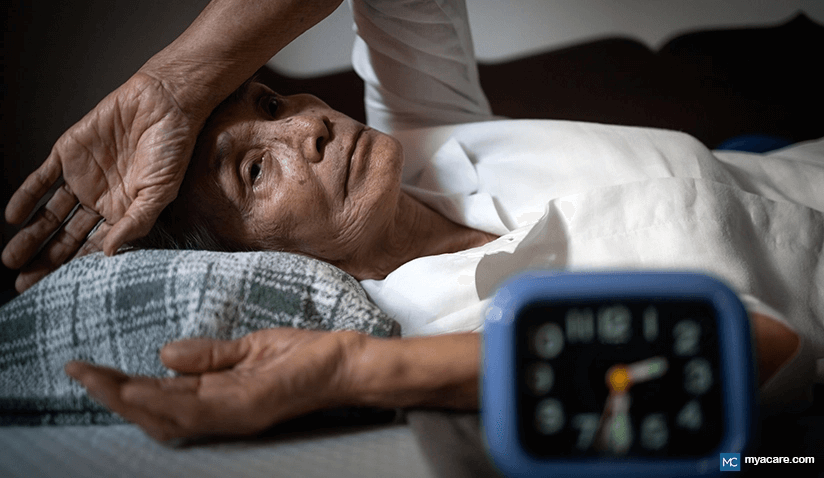
The inability to initiate or maintain sleep is known as insomnia. Older adults (aged more than 56 years) are more likely to suffer from insomnia and take more time to fall asleep than younger adults.
Older adults suffering from insomnia or other sleep difficulties are at a higher risk of developing memory problems, experiencing day time fatigue, and suffering from depression. In some cases, the COVID 19 situation has caused this group to be forced to live in isolation and caused them to worry about their health, adding to stress and increasing the likelihood of insomnia. Therefore it is important to understand the causes and ways to treat insomnia.
Prevalence:
The prevalence of insomnia is reported to be more than 30% in the US, with the incidence increasing to more than 50% in older adults. Women are two times more likely to have insomnia than men.
About 23% of older adults with insomnia have an increased risk of developing depression.
Changes in the Sleeping Pattern in Older Adults
A normal sleep cycle comprises of 3 segments:
- Light sleep
- Deep sleep (or non- rapid eye movement, NREM): This is considered to be the most soothing part of sleep
- Rapid eye movement sleep (REM): This is important for learning and retaining memory
Deep sleep (NREM) is observed in the first half of sleep and REM in the second part. Usually it takes 1.5-2 hours to shift from NREM to REM stage of sleep.
Older adults may experience difficulty in following this sleeping pattern, caused by the following changes:
- Changes in the circadian rhythm which regulates individuals’ sleep-wake cycle
- Difficulty in initiating sleep
- Reduction in NREM which results in fragmented sleep and frequent awakenings
- A decline in REM sleep which leads to difficulty in remembering things
These changes affect the duration and quality of sleep in older adults. With aging, the time taken to fall asleep (sleep latency) increases, which makes them feel tired and exhausted more easily. It also increases their urge to take frequent naps during day time.
Causes of sleep disorders include:
- Disturbance in circadian rhythm: A circadian rhythm is the body’s internal process which repeats every 24 hours and regulates the body’s activities, including sleep patterns. With aging, a disturbance in the circadian rhythm may cause changes in the sleep pattern. These changes are more prominent in individuals who suffer from ailments such as sleep apnea (breathing halts and starts throughout the night), restless leg disorder (a condition with greater urge to move legs), and advanced sleep phase syndrome (continuous pattern of sleeping and waking up early), leading to insomnia.
- Stress: Stress due to financial issues, physical disability, loneliness, or loss of family and friends also places individuals at an increased risk of developing insomnia. The spread of COVID-19 has increased the risk of stress in older adults. The stress is not just due to higher death risk but also due to self-isolation and restrictions imposed to control the spread of the disease.
Research suggests that the fear of developing an infection, long duration of quarantine, prohibited social interactions, boredom, inadequate supplies of essentials, unpredictability about the disease, and financial losses have affected the psychological health of a large section of individuals. Lack of social and physical contact and a sense of loneliness have also led to grief, sorrow, numbness, anger, frustration, and anxiety-related insomnias.
- Presence of illness: Older adults are more prone to various chronic cardiovascular diseases, lung conditions, gastrointestinal conditions, kidney, psychiatric, menopause, arthritis, and nervous system related disorders. Most of these physical disorders are painful and interfere with sleep.
- Medications: Prolonged use of medications such as antidepressants, stimulants of the central nervous system and cardiac disorders, and bronchodilators (for dilation of breathing passage) can cause sleep-related problems.
- Lifestyle habits: Various lifestyle and sleep-related habits such as hitting the bed early, using the bed for different activities (e.g., reading, watching TV), use of electronic devices while lying on the bed, and intake of heavy meals just before hitting the bed can impact the sleep cycle. Other lifestyle choices such as smoking, alcohol consumption, and lack of physical activity with a sedentary routine can also affect the sleep cycle.
- Environmental factors: Excessive noise, insufficient exposure to sunlight, extreme temperatures, and uncomfortable bed are other factors that can impact sleep.
How Does Insomnia Impact Life?
Insomnia impacts the physical and mental health of older adults, reducing the overall quality of life. Older adults complain of symptoms such as difficulty in falling asleep, disturbed night sleep, frequent waking up in the night, excessive day time sleepiness, day time fatigue, frequent anxiety, and irritability.
Decreased sleep quality can also lead to a decrease in memory and concentration levels, make the older adults prone to accidents, and weaken their cognitive abilities. Research suggests that it is also associated with a higher rate of mortality in older adults.
Treatment of insomnia:
- Non-medical therapy: There are several measures which can help treat insomnia in older adults. These measures should be continued even while undergoing medical therapy.
Things to follow
- Walk or exercise during mornings or early evenings
- Go to bed only when sleepy
- Maintain a comfortable room temperature
- Observe the effect of medicines on sleep
- Maintain a fixed schedule to rest, sleep, eat, and exercise
- Include relaxing exercises such as meditation, breathing exercises, muscle tensing, and relaxing exercises in your regime
Things to avoid
- Mental stress
- Day time napping
- Exposure to noise and lights while sleeping
- Heavy meals before hitting the bed
- Reading or using gadgets sitting on bed
- Consumption of alcohol, caffeine, and cigarettes
- Intake of excessive liquids in the night as it may increase the urge to urinate and disturb sleep
- Medical therapy: Medical therapy: In advanced cases of insomnia, the doctor will prescribe medications based on symptoms and severity. Medications may be prescribed to improve the quality of sleep and decrease the time taken to initiate sleep. Antihistamines, which are used to treat allergies and cough, can also induce sleep. Due to the presence of side effects on prolonged use, medications should only be taken under strict medical guidance. These medications should be discontinued in a gradual progression to avoid any rebound effect.
- Herbal therapy: Use of herbal medications such as valerian, chamomile, kava-kava, and passion flower are helpful in insomnia. However, little scientific evidence is available to support this therapy.
To search for the best Neurology Healthcare Providers in Croatia, Germany, India, Malaysia, Spain, Thailand, Turkey, Ukraine, the UAE, UK and the USA, please use the Mya Care search engine.
To search for the best healthcare providers worldwide, please use the Mya Care search engine.

Dr. Shilpy Bhandari is an experienced dental surgeon, with specialization in periodontics and implantology. She received her graduate and postgraduate education from Rajiv Gandhi University of Health Sciences in India. Besides her private practice, she enjoys writing on medical topics. She is also interested in evidence-based academic writing and has published several articles in international journals.
Sources::
Featured Blogs



