Latest Advances in the Treatment of Cervical Spine Degeneration

Neck pain is among the most common symptoms of cervical spine degeneration in which the neck discs become dry and shrink with age. Studies estimate a prevalence of 60% in people over 40 as compared to 25% in those under 40.
Neck pain from cervical disc disease is often managed with medication, including over-the-counter painkillers, anti-inflammatory medication, steroids, narcotic pain killers, and cortisone pills. Heat and cold therapies, physical therapy, weight loss, and chiropractic adjustments can also help relieve neck discomfort from disc degeneration.
Spinal surgery may be recommended if the pain in the neck persists or neurological symptoms, such as tingling and muscle weakness, arise. Surgical options for cervical spine degeneration include cervical rhizotomy, laminectomy, disc fusion, cervical discectomy, and artificial disc replacement.
What Is Cervical Spine Degeneration?
Cervical spine degeneration, or cervical spondylosis, is a term used to describe the wear and tear of the spinal discs in your neck that happens with age.
Degenerative disc disease is a prevalent condition and is the most frequent cause of neck stiffness and brachialgia.
Cervical spine degeneration can be severe without displaying symptoms, leaving patients unaware of their condition. Sometimes, cervical disc degeneration can affect the nerves in the neck and cause the following symptoms:
- Pain in the neck and the muscles next to the neck (trapezius muscles)
- Pain between the shoulder blades
- Pain radiating down the arm to the hand, wrists, and fingers
- Tingling and numbness (paresthesia) in the arms or fingers. The paresthesia usually comes and goes and generally does not last unless the nerve becomes damaged.
- Rarely, weakness in the legs, difficulty walking, trouble with bowel or bladder control.
What causes cervical spine degeneration?
The spine comprises bones called the vertebrae with soft spacers between them called discs. Your spine can be divided into three regions:
- The region in your neck (cervical spine)
- The region in your chest (thoracic spine)
- The region in your lower back (lumbar spine)
The primary support of your neck comes from your cervical spine – consisting of 7 vertebrae separated by six discs.
The vertebrae are made of hard bone that gives the spine its rigidity and allows humans to stand up. The discs are tough and firm on the outside, but on the inside, they are filled with a softer, jelly-like substance that acts as a shock absorber.
Discs are essential for the functioning of the cervical spine in your neck because they provide it with cushioning, support, and range of motion.
The aging process affects cervical spine degeneration. As you get older:
- The soft part inside the neck discs may begin to dry up and the outer part of the disc begins to collapse.
- The discs in your neck become brittle because of moisture loss and begin to lose their cushioning effect.
- This allows the vertebrae on either side of the disc to get closer together and become compressed.
- In response, the spine may produce extra bone in an attempt to strengthen itself. This can lead to the formation of bony growth known as spurs.
- Over time, the bone spurs may begin to pinch the spinal nerves in the neck that lead to your arms which can cause pain, tingling, and weakness.
It is still not exactly clear why the degeneration of the neck discs happens. Doctors suspect that it may develop over time because of:
- Natural history of arthrosis
- Excessive lifting
- An injury to the spine
- A family history of spine issues
Leading centers use innovative and advanced testing methods, such as electromyography (EMG), nerve conduction study (NCS), multiparametric magnetic resonance imaging (MRI), and computed tomography (CT) scans, to evaluate the nerves and muscles and to determine the severity of degeneration in the cervical spine.
Conservative Treatment of Cervical Spine Degeneration
For neck pain from cervical degenerative disc disease, your doctor will likely recommend self-care and non-surgical treatment options to manage your discomfort effectively.
Home remedies for neck stiffness and soreness
If the degeneration of your cervical discs is only causing stiffness and soreness in your neck, the following self-care remedies can be used:
- Heat and cold therapies: Applying an ice pack or a heated gel pack to the affected areas can help relieve mild neck stiffness and pain.
- Physical therapy: Most non-surgical neck treatment options include exercise or stretching. A physical therapist or a trained health professional can prescribe an exercise regimen incorporating stretches to increase the strength and flexibility of your neck and reduce discomfort.
- Rest: Neck soreness and stiffness can be decreased by avoiding activities that strain the neck, such as hunching over a computer screen, driving for long hours, and certain physical activities that exert the neck (swimming, heavy lifting).
- Maintaining a strong posture while sitting or standing – Do not slouch your neck or shoulders.
- Weight loss: Excess weight can stress the spine and pull the spinal vertebrae and discs out of alignment. Losing weight can relieve some of the additional pressure on the cervical discs and help with neck and shoulder pain.
- Chiropractic adjustment: A chiropractor or other health professional can manually adjust the cervical spine to improve your neck’s range of motion and reduce pain.
Medication to treat chronic cervical neck pain
If the pain in your neck persists and becomes chronic, your doctor may recommend the following:
- Over-the-counter (OTC) pain relievers: Acetaminophen (Tylenol) and ibuprofen (Advil, Motrin) are usually the first-line drug treatments for neck pain. To ensure the safe use of acetaminophen and other pain relievers, stick to the label suggestions and your doctor’s recommendations.
- Non-steroidal anti-inflammatory drugs (NSAIDs): NSAIDs, such as aspirin, can help both ease your neck pain and reduce inflammation. Many NSAIDs are available OTC. Nevertheless, they also need to be taken with care, especially when used for a long time.
- Narcotic pain killers: These may be prescribed for severe neck pain that won’t go away with other types of painkillers. Since these prescription painkillers can become addictive, they are usually prescribed for a short time under a doctor’s guidance.
- Oral steroids: Steroids such as prednisone can help decrease the inflammation and pain in your neck.
- Steroid injections: Steroids for neck pain can be delivered directly to a certain part of the neck using X-ray guidance. Steroid injections in the neck, such as cervical epidural steroid injections and cervical facet injections, are effective in reducing cervical neck pain.
- Muscle relaxants: Prescribed medications, such as Baclofen, can relax tightened muscles around the neck and alleviate some neck pain.
- Cortisone pills: For severe neck pain that is not relieved by other medications, small doses of cortisone may be prescribed for a short period.
Anticonvulsants are sometimes used off-label to treat nerve-related neck pain. Nonetheless, it is still not clear how anticonvulsants work on cervical spine pain, and their use may lead to severe side effects.
Surgical Treatment of Cervical Spine Degeneration
A surgical solution may be recommended in rare cases where the cervical spine degeneration symptoms resist conservative treatments.
Surgical treatment for neck disc degeneration may be done in case of:
- The presence of neurological symptoms such as persistent arm numbness/weakness, trouble walking, and bowel problems. Neurological symptoms indicate a risk of permanent nerve damage. Therefore, surgery may be recommended to alleviate pressure on the nerve.
- Severe chronic pain that makes regular daily activities challenging and is not adequately relieved after months of non-surgical treatment.
Minimally invasive surgical techniques and other advanced procedures can reduce the risks associated with spine surgery and speed up recovery.
1. Cervical Rhizotomy
A cervical rhizotomy is a minimally invasive procedure for chronic neck pain with swollen and symptomatic facet joints. It involves severing or destroying specific nerve fibers that transmit pain signals from the inflamed facet joint, thereby blocking pain signals from reaching the brain. Cervical rhizotomy can be performed using radiofrequency ablation, chemicals (glycerin/glycerol), or minimally invasive endoscopic surgery. The procedure is performed on an outpatient basis and does not require hospitalization; patients are allowed to return home the same day. Cervical rhizotomy usually provides immediate pain relief with effects lasting up to several years till the nerve repairs itself.
2. Laminectomy (decompression surgery)
A laminectomy, or decompression surgery, is a surgery that removes the back part of the vertebrae (the lamina) which covers the cervical spinal canal.
As a result, the spinal canal is enlarged and the pressure on the spinal cord and nerves is reduced.
Typically requiring a one day hospital stay, same-day discharge is possible in some cases of laminectomy.
3. Cervical disc fusion
Cervical spine fusion is a surgery for permanently connecting two or more vertebrae in your cervical spine to prevent them from moving abnormally.
Recently, innovative fusion techniques have been developed that mimic the normal healing process of broken bones. During spinal fusion:
- Surgeons place a bone or bone-like material between two neck vertebrae.
- Metal plates, screws, and rods may be used to hold the vertebrae together.
- The vertebrae eventually heal together into one solid unit.
- Consequently, the fused neck vertebrae improve spine stability and reduce neck pain.
4. Anterior cervical discectomy and fusion (ACDF)
If there are neurological symptoms caused by spinal cord compression, surgeons may include the removal of a neck disc in your cervical fusion surgery. This will create more space for the spinal cord and relieve pressure on the nerves before the spinal fusion is done.
This type of spine surgery is known as anterior cervical discectomy and fusion (ACDF) surgery. During an ACDF:
- An incision is made through the front of the neck
- The problematic disc is carefully removed
- The pressured nerve root is decompressed
- A metal cage device or bone graft is then inserted between the vertebrae (cervical fusion) to help maintain or regain the normal height of the disc space.
5. Cervical disc arthroplasty (artificial disc replacement)
Disc fusion may stiffen part of your spine and change the way it moves, causing additional stress and strain on the neck vertebrae. This can increase the rate of spinal degeneration. Consequently, neurosurgeons may perform an advanced spinal surgery called cervical disc replacement as an alternative to cervical disc fusion.
Cervical artificial disc replacement is a joint replacement procedure (arthroplasty) that replaces a natural cervical spine disc with an artificial cervical disc.
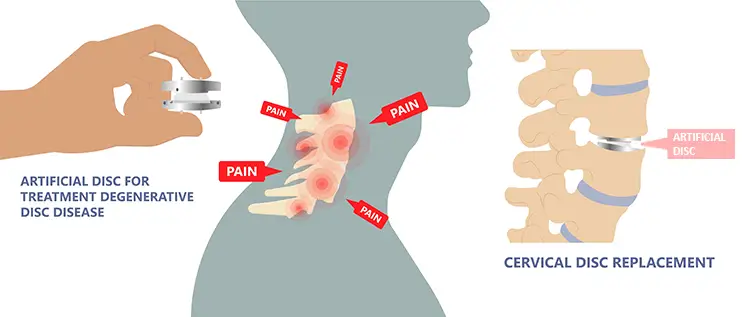
During cervical disc replacement:
- Surgeons will skillfully remove the damaged natural neck disc
- A prosthetic neck disc is then inserted instead of it in the intervertebral space (between the two vertebrae)
- The inserted disc essentially functions like a joint, allowing flexion, rotation, extension, and side bending of the neck spine
Artificial neck disc replacement surgery is performed to preserve motion at the spinal level, improve flexibility in the neck, and relieve neck pain.
Summary
Cervical neck surgery can be successful in relieving pressure on the nerve roots or the spinal cord, therefore, reducing neurological symptoms such as arm pain, tingling, or weakness. However, pain specific to the neck can often be managed with various non-surgical remedies and treatment options.

Dr. Jesús Lafuente is the head of neurosurgery at the Hospital Universitari Sagrat Cor in Barcelona, Spain. His special interests include skull base neurosurgery, chiari and syringomyelia, spinal deformity, spinal tumors, degenerative disease, and performing surgeries in developing countries. Dr. Lafuente is an Associate Professor in Neurosurgery at Universidad Autónoma of Barcelona. Having authored 35 publications, 9 book chapters, 3 editorial letters, and 195 personal presentations, he currently reviews the National Spanish Neurosurgical journal, Acta Neurochirurgica, Brain & Spine Journal, World neurosurgery and the European spine journal. In 2003, he received the prestigious "Mario Boni Award" for the best research paper at the Congress of the European Society for Cervical Spine Research (CSRS).

Hospital Universitari Sagrat Cor (Sagrat Cor University Hospital) is a privately held center that offers all medical-surgical specialties employing around 1,100 professionals. The center is accredited as a teaching hospital by the Faculty of Medicine of the University of Barcelona and the Ministry of Health and Consumer Affairs. Other Catalan and foreign universities affiliate with Hospital Universitari Sagrat Cor for undergraduate and postgraduate training. The neurosurgery team at the Hospital Universitari Sagrat Cor, led by Dr. Jesus Lafuente, is highly trained in diagnosing and treating degenerative cervical spine disease. The spine and neurological surgery experts at the hospital collaborate in performing minimally invasive surgical procedures and techniques to correct problems in the spine.
Sources:
Featured Blogs



