Plantar Fasciitis – Treatment Options and the Role of Stem Cell Therapy

Medically Reviewed by Dr. Sony Sherpa, (MBBS) - September 23, 2024
Plantar Fasciitis is the most common cause of chronic heel pain, Pain caused by plantar fasciitis may persist for several weeks to a year in most patients. Plantar Fasciitis treatment options can help reduce pain and speed up the recovery process. Research into cellular mechanisms has highlighted the key role of stem cell therapy in treating Plantar Fasciitis.
The article below provides an overview of Plantar Fasciitis, including symptoms, causes, risk factors, and treatment options.
What is Plantar Fasciitis?
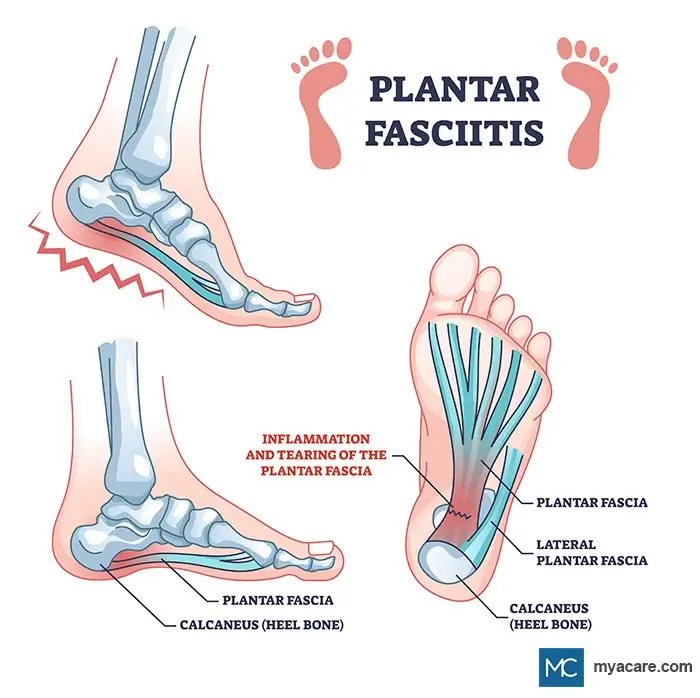
When the plantar fascia of the feet become irritated, inflamed, and painful, it is known as Plantar Fasciitis. Ultrasonography often reveals microtears, granulation of tissue, disordered collagen, and other signs of plantar fascia degeneration. Plantar Fasciitis is curable in over 95% of cases.
The condition usually lasts for several months to a year, with most cases resolving after this time. Treatment can help to manage symptoms and, in some cases, may be required for resolution.[1]
Anatomy. The plantar fascia are ligaments that lie just beneath the skin under the feet, spanning from the heel to the forefoot. They are involved in supporting the arches of the feet and are required for optimal balance and movement while standing and walking. In addition to aiding the alignment of the feet, they serve as shock absorbers and limit foot strain.
Symptoms. The primary sign of Plantar Fasciitis is a sharp pain that radiates from under the heel. The pain is often the worst while taking the first few steps in the morning. Walking and gently stretching the area helps to alleviate the pain, yet it tends to get progressively more tender as the day wears on. Flexing the feet and prolonged standing throughout the day can promote pain, and in severe cases, prolonged sitting can as well.
Causes. Regarded as an overuse injury, Plantar Fasciitis is caused by excessive strain and wear and tear of the plantar fascia. It may also occur as a result of a direct injury. While injury can cause acute inflammation, persistent Plantar Fasciitis is not thought to arise from chronic inflammation. Continuous strain on the plantar fascia promotes thickening, stiffening (fibrosis), elasticity loss, and degeneration of the tissue, which gives rise to chronic pain. Other studies highlight unbalanced stem cell proliferation between stem cell types (vascular and collagen-related stem cells) and over-vascularization of the area, resulting in a continuous cycle of destruction, “regenerative” overgrowth, irritation, and pain[3]. Resolution depends upon the ability of the tissue to regenerate properly in a balanced manner.
Risk Factors. Advanced age, regular and competitive running, certain types of dance, obesity, poor posture, heel pad atrophy, prolonged standing, and weight-lifting are all common risk factors. Unusual foot alignment, flat feet, or a high arch can also place strain on the plantar fascia. Approximately 50% of those with Plantar Fasciitis present with heel spurs as well. They are not known to cause Plantar Fasciitis, yet may increase the strain on the plantar fascia.
Prevalence. Plantar Fasciitis is the most common cause of heel pain, estimated to affect roughly 10% of the global population and account for 1-2 million patient visits annually.
Plantar Fasciitis Treatment Options
Plantar Fasciitis treatment options are similar to those for general tendinitis. These include:
- Gentle Calf and Feet Exercises. Carefully stretching the area along the surrounding tissues can help ease stiffness and reduce pain. Studies also highlight that these exercises are critical for recovery, even with other treatments. The plantar fascia-specific stretch has been shown to be the best for improving daily functionality and lowering pain. It involves using one hand to flex the toes as upright as possible while using the other hand to gently palpate or gently sink fingers into the plantar fascia (the tissue just after the heel in the arch of the foot). Holding the stretch for 30 seconds, three times per session, is optimal to perform after getting out of bed and after prolonged sitting. The calves can also be stretched for an even better result. Speak to your doctor for more specific information on exercises for Plantar Fasciitis recovery.
- Ice Massage. A fluid-filled frozen can or bottle can help massage the arch of the foot and manage pain. This can be achieved by standing on the bottle and rolling it under the affected foot for 5-10 minutes at the end of each day. This is known to enhance foot functionality and helps to improve the patient’s ability to exercise the feet.[4]
- Orthopedic Support. Heel pads, orthopedic insoles, and night splints are thought to offer better support, limit the motion of the affected area, and lower pressure. Some studies suggest that these are as effective as a placebo and unnecessary[5], while others suggest that combining full-length insoles with rocker shoes or night splints may be beneficial.[6] Some patients with Plantar Fasciitis find relief with compression stockings, which might help by interrupting the overgrowth of blood vessels, lowering pain, and helping the patient perform fascia exercises.[7]
- NSAIDs can help to manage pain, thin the blood, and reduce inflammation in the first month after injury to the fascia, yet are likely to be less effective after the initial injury phase. Due to negative side effects, it is advisable to limit their use.
While the above measures often help to resolve Plantar Fasciitis, the recovery process is long and can still be rather painful for those with severe cases. Several techniques have been developed to help manage pain and speed up recovery of the plantar fascia, the most promising of which would be stem cell therapy.
Despite the benefits, other therapeutic options only offer short to medium-term benefits over performing daily plantar fascia exercises. While they may enhance regeneration, strengthening the fascia is still the most important part of recovery.
Injections for Plantar Fasciitis
Foot injections for Plantar Fasciitis treatment are very popular treatment options that often speed up the recovery process by several months and substantially improve the pain intensity. Of all the below injection options, PRP for Plantar Fasciitis often gives the best results.
- Platelet-Rich Plasma (PRP) Injections. Platelet-rich plasma injection is a regenerative technique used to stimulate regeneration and new growth in a damaged or under-functioning area of the body. It involves taking a blood sample from the patient, concentrating the platelets 5-10 times by centrifugation, and then re-injecting them back into the area requiring treatment[8]. The blood platelets do more than seal wounds through clotting and are able to release neurotransmitters and other signals that substantially enhance regenerative processes. PRP for Plantar Fasciitis can help mobilize vascular stem cells to the area and stimulate the repair of the damaged plantar fascia. This is thought to be more effective than other treatments as it counteracts degeneration with minimal side effects. Preliminary evidence suggests it can provide pain relief in the long run, reduce the need for additional treatment[9], and greatly enhance the efficacy of all other treatment options.[10]
- Stem Cell Injections for Plantar Fasciitis. Another popular treatment for reducing pain and promoting optimal regeneration is stem cell therapy.[11] While stem cell transplantation may improve healing and lower pain for many other ligament injuries[12], one study suggests that Plantar Fasciitis could develop or become worse after transplantation, especially in those receiving treatment for hematologic cancers[13]. This is likely due to the risk of transplant rejection or graft vs. host disease, both of which can exacerbate pain and inflammation. In this regard, indirect stem cell therapy may be superior, such as PRP injections. Other studies suggest that amniotic tissue transplantation (high in stem cells with low rejection risk) may help to almost completely negate heel pain in those with Plantar Fasciitis after 12 weeks.[14]
- Steroid Injections. Patients resistant to all other treatment options may find that corticosteroid injections can help in lowering pain in the affected area for several weeks after treatment. This is known to be effective in reducing inflammation in the area. However, it is not recommended for most cases of Plantar Fasciitis, which are indicative of chronic degeneration rather than chronic inflammation. More than one injection is not advisable due to the elevated risk of heel pad atrophy and/or rupture, which can perpetuate the condition and delay recovery.
- Injection Techniques: Ultrasound-Guided vs. Palpation-Guided. Ultrasound-guided PRP injections proved to be superior to palpation-guided injections. This is due to better accuracy as well as improved breakdown of faulty and stiff plantar fascia tissues.[15]
Complementary Therapy for Plantar Fasciitis
Aside from foot injections for Plantar Fasciitis, other therapies are available that may complement the recovery process:
Extracorporeal Shockwave Therapy (ESWT) makes use of low-frequency, high-energy ultrasound to break down overgrown and stiff fibrotic areas of the plantar fascia, as well as promote optimal stem cell mobilization and regeneration. The long-term results were shown to be of similar efficacy to that of PRP for Plantar Fasciitis[16]. Unlike PRP, ultrasound was shown to promote collagen repair, which suggests that it can stimulate a different population of stem cells to that of PRP (which largely promotes vascular stem cells and not those found in connective tissues). Due to the way in which ESWT disrupts abhorrent growth processes and how PRP encourages optimal stem cell function, combining both therapies with gentle fascia exercises may be the best technique for reducing pain and speeding up recovery.
Acupuncture and Dry Needling. Very limited evidence is available to suggest a short-term pain relief of acupuncture and/or dry needling on pressure points associated with the heel[17]. Results suggest the benefits are best utilized within the first 8 weeks of Plantar Fasciitis onset.
When is Surgery for Plantar Fasciitis Necessary?
Surgery is often only deployed for around 5% of those with Plantar Fasciitis when the condition does not see resolution after a year and with intensive non-invasive treatment. All surgeries offered for Plantar Fasciitis aim to decrease tension on the plantar fascia and include:
- Partial plantar fascia release is often an open surgery in which a small incision is made in the plantar fascia to reduce tension and remove potential bone spurs.
- Gastrocnemius recession is a surgery in which the calf muscles are lengthened to allow for better movement and flexion of the feet while reducing pressure on the plantar fascia. This surgery is often done together with the above surgery for full relief.
Despite being well-tolerated in most cases, it may cause chronic heel pain and/or nerve damage and should only be opted for as a last resort if other treatment options fail. In the event of surgery, one may wish to consider complementary stem cell therapy, such as PRP, to enhance outcomes and lower the risk of complications.
Conclusion
The best remedy for Plantar Fasciitis involves gentle exercises to strengthen the area and manage painful symptoms. The mechanisms underlying the condition pertain to faulty regenerative processes that cause excessive growth, stiffness, and degeneration of the plantar fascia, rendering typical anti-inflammatory treatment options unnecessary (e.g., steroid injections and NSAIDs). PRP for Plantar Fasciitis shows the most therapeutic promise as it is able to improve the regenerative responses, lower pain, and enhance all other treatment options without side effects. Ultrasound treatments like ESWT can further speed recovery times by interrupting degenerative processes, increasing collagen repair, and regulating regeneration. Surgery should only be a last resort if treatment and exercises prove ineffective after 12 months. PRP may help lower the risk of surgical complications.
To search for the best Orthopedics Healthcare Providers in Croatia, Germany, India, Malaysia, Singapore, Spain, Thailand, Turkey, the UAE, UK and the USA, please use the Mya Care search engine.
To search for the best doctors and healthcare providers worldwide, please use the Mya Care search engine.
The Mya Care Editorial Team comprises medical doctors and qualified professionals with a background in healthcare, dedicated to delivering trustworthy, evidence-based health content.
Our team draws on authoritative sources, including systematic reviews published in top-tier medical journals, the latest academic and professional books by renowned experts, and official guidelines from authoritative global health organizations. This rigorous process ensures every article reflects current medical standards and is regularly updated to include the latest healthcare insights.

Dr. Sony Sherpa completed her MBBS at Guangzhou Medical University, China. She is a resident doctor, researcher, and medical writer who believes in the importance of accessible, quality healthcare for everyone. Her work in the healthcare field is focused on improving the well-being of individuals and communities, ensuring they receive the necessary care and support for a healthy and fulfilling life.
Sources:
Featured Blogs



