Post-COVID-19 Rehabilitation at Medical Park

 |
“COVID-19 patients not only suffer from long-term damage of the lungs, but show signs of heart muscle inflammation, neurological or psychiatric diseases. I consider post-COVID-19 rehabilitation necessary as it is offered by Medical Park.” "Prof. Dr. med. Martin Halle" Medical Director Specialist in internal medicine, cardiology and Sports Medicine Technical University of Munich |
COVID-19 - A Multifaceted Disease
Medical Park premium rehabilitation hospitals are specialists in prevention and post-operative rehabilitation.
COVID-19 is a multifaceted disease that needs aftercare. Post-COVID-19 care has become a new treatment field of medical rehabilitation and is now available at Medical Park.
The German healthcare system enjoys an excellent reputation and has managed the outbreak of COVID-19 well. Germany’s healthcare sector is far advanced and provides a unique structure of cooperating acute and rehabilitation hospitals, thus ensuring great treatment results for each individual.
The symptomatic course of COVID-19 primarily affects the respiratory tract. Meanwhile it is well known that organs such as the heart, the brain, the peripheral nervous system, and the musculoskeltal system are often affected by COVID-19. Such “multiorgan” manifestation of COVID-19 is often seen in severely affected patients. Even when laboratory findings indicate that the disease is overcome, many patients report residual symptoms like dyspnea, heart discomfort, arrhythmias, a variety of neurological disorders and psychological phenomena like anxiety and depression. Inter-individual prevalence and degree of these symptoms show considerable variability.
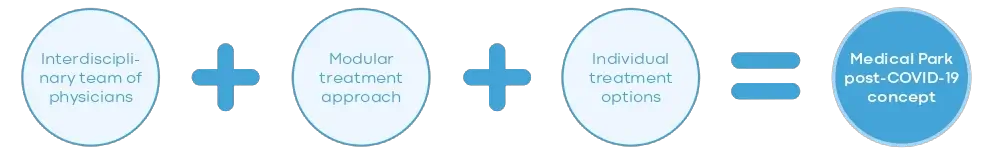
Head physicians of the Medical Park rehabilitation hospitals constituted a “post-COVID-19 rehabilitation board” and developed a modular rehabilitation concept for post-COVID-19 patients.
Facts
- Established in 1977
- 14 premium hospitals in Germany
- 70,000 patients admitted per year3,100 beds
- 3,500 staff members
Areas of Treatment:
- Neurology (including ICU)
- Psychosomatics
- Orthopaedics/traumatology/sports medicine
- Internal medicine/cardiology
- Oncology
Interdisciplinary Modular Rehabilitation After Covid-19:
The course of treatment is structured as a “Basic” and “Additional” module for the fields of “internal medicine/ cardiology”, “neurology”, “orthopaedics” and psychosomatic medicine with a duration of 14 and 7 days, respectively.
Upon referral by the “post-COVID-19 rehabilitation board”, each patient is assigned to a “Basic” module and to “Additional” modules as required. The joint recommendation is based on individual patient needs, identified by leading symptoms and underlying diagnoses apart from COVID-19.
Treatment Modules
Based on the individual needs of the patient, assessed in the basic module.
- Type of residual post-COVID symptoms
- Underlying (non-COVID) diagnoses
| Internal Medicine Cardiology | Neurology | Orthopaedics | Psychosomatic Medicine and Psychotherapy | ||
| Head Physician | Prof. Firschke. | Prof. Young |
Prof. Schmitt-Sody |
Dr. Menke |
|
|
Diagnostics |
|
|
|
|
|
| Therapy |
|
||||
INTERDISCIPLINARY POST-COVID-19 REHABILITATION BOARD

“Severe COVID-19 pneumonia can lead to structural and haemodynamic changes in the lungs and the heart (pulmonary fibrosis, pulmonary hypertension, right heart failure). Training-based rehabilitation can significantly improve maximum oxygen uptake and enhance cardiopulmonary performance.”
Christian Firschke
MD, PHD, FESC, FACC, MHBA
- Professor of Internal Medicine/Cardiology
- Technical University of Munich, Germany
- Head of Cardiology, Medical Park St. Hubertus, Bad Wiessee, Germany
- Consultant, cardiac surgery, German Heart Centre Munich, Germany
- Trained at Technical University of Munich, Germany and University of Virginia, U.S.A.
- Fellow of the European Society of Cardiology
- Fellow of the American College of Cardiology

“The clinical picture after severe pneumonia with intensive care therapy is characterised by a general muscle weakness and muscle wasting causing long lasting immobility, respiratory weakness and sensory disturbances, so called ICU acquired weakness. Our concept takes all these aspects into account and offers best support to regain health.”
Peter Young
MD, PHD
- Professor of Neurology and Neurogenetics
- Westfälische Wilhelms-Universität, MÜNSTER, Germany
- Head of Neurology, Medical Park Bad Feilnbach, Reithofpark, Germany
- Trained at Westfälische Wilhelms-Universität, MÜNSTER and Eidgenössische Technische Hochschule (ETH) Zurich, Switzerland
- Specialisation in neurology, neurogenetics, intensive care medicine and sleep medicine
- Board member of the German Sleep Society (DGSM) and the German Muscle Society (DGM)

“We support patients in regaining their independence after a COVID-19 pneumonia. We focus on the long-term wellbeing of our patients.”
MD, PHD
- Professor of Orthopaedic Surgery
- Ludwig-Maximilians-Universität Munich, Germany
- Head of Orthopaedics, Medical Park Chiemsee, Medical Park Prien Kronprinz, Germany
- Specialisation in sports medicine and chirotherapy
- Board member of the German Knee Society (DKG)
- Trained at Ludwig-Maximilians-Universität Munich, Germany

Andreas Menke
MD, PHD, ASSOC.-PROF.
- Head of Psychosomatic Medicine and Psychotherapy, Medical Park Chiemseeblick, Bernau-Felden, Germany
- Associate Professor of Psychiatry and Psychotherapy at Ludwig-Maximilians-Universität Munich, Germany
- Member of the Comprehensive Heart Failure Center Germany, University Hospital of WÜRZBURG, Germany
- Member of the Graduate School of Life Sciences (GSLS), Julius-Maximilians-Universität WÜRZBURG, Germany
- Trained at Ruprecht-Karls-Universität Heidelberg, Germany
We offer the treatment in four of our hospitals:
- Medical Park St. Hubertus
- Medical Park Reithofpark
- Medical Park Chiemsee
- Medical Park Chiemseeblick.
Featured Blogs



