The Latest in Advanced Management of Deep Infiltrating Endometriosis
What Is Deep Infiltrating Endometriosis?
How Is Deep Infiltrating Endometriosis Diagnosed?
What Are The Challenges Of Managing Deep Infiltrating Endometriosis?
What Are The Advancements in Managing Deep Infiltrating Endometriosis?
Deep infiltrating endometriosis is an advanced type of endometriosis that can cause pain and infertility. Studies estimate a prevalence of endometriosis in 10% of females of reproductive age, whereas the incidence of deep endometriosis is roughly 1 - 2%.
There is no cure for deep endometriosis, and the treatment focuses on improving the symptoms and minimizing complications.
Recently, advances in deep infiltrating endometriosis management helped surgeons decrease the risk of complications and increase fertility. Those advancements include PlasmaJet surgical devices, indocyanine green (ICG) fluorescence, and stenting during partial cystectomy.
Utilizing the latest advancements in managing this highly invasive disease, specialized centers adopt a multidisciplinary approach involving gynecologists, fertility experts, surgeons, and radiologists to treat endometriosis-associated pain and preserve fertility.
What Is Deep Infiltrating Endometriosis?
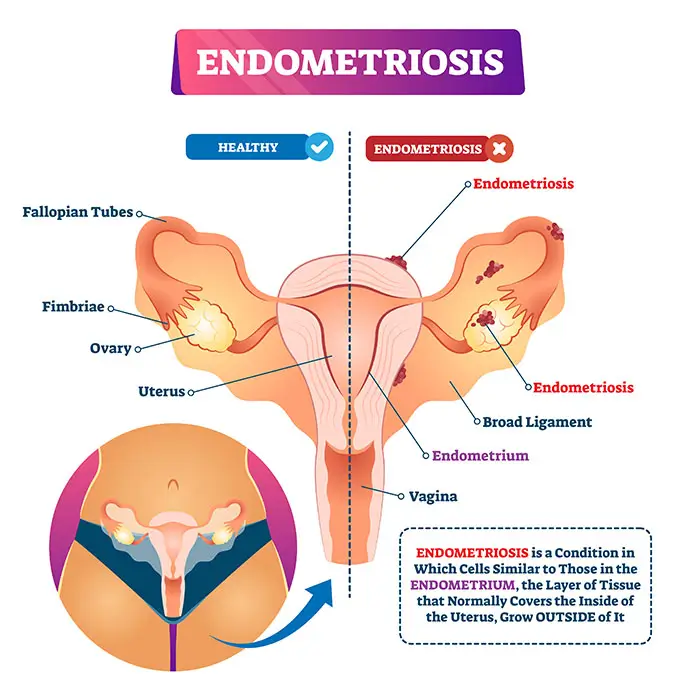
Endometriosis happens when the tissue lining the uterus (endometrium) grows outside the uterine cavity.
Even when outside the uterus, the endometrial tissue behaves as it usually does inside the uterus – it breaks apart and starts bleeding during the menstrual period.
The extent of endometriosis is measured according to the depth and spread of the endometrial tissue and other organs affected. The American Society of Reproductive Medicine outlines four endometriosis stages:
- Stage 1 - Minimal
- Stage 2 - Mild
- Stage 3 - Moderate
- Stage 4 - Severe
Most women have minimal or mild endometriosis, defined by shallow implants and minor adhesions. Chocolate cysts and more extensive adhesions are associated with moderate and severe endometriosis stages. Many women are concerned about the question - can endometriosis cause infertility? It is important to note that there is no relationship between the stage of endometriosis and the presence or intensity of symptoms. However, infertility or difficulty in conceiving is more likely with stage 4 endometriosis.
Nevertheless, the numbered stages can be deemed inadequate in providing insights into the numerous possible variations, the patient’s pain or the location of lesions. Therefore, the Endometriosis Foundation of America proposed descriptive categories based on the anatomical location of endometriosis within the pelvic and abdominal cavities. The different types of endometriosis based on this classification are:
- Superficial endometriosis (Peritoneal endometriosis) is the most common type of endometriosis. Lesions appear on the surface of organs outside the endometrium and closer to the abdominal and pelvic cavities.
- Ovarian endometriomas are dark cysts, also called chocolate cysts, that develop in the ovaries because of endometriosis. They are filled with menstrual blood and don’t respond well to treatment.
- Deep infiltrating endometriosis is an advanced form of endometriosis. The endometrial tissue spreads deeper into the pelvic organs, more than 5 millimeters deep. Deep infiltrating endometriosis can affect the ovaries, rectum, uterus, and even result in “frozen pelvis”, a condition where the pelvic organs develop extensive adhesions to one another. More severe cases can involve organs both inside and outside the pelvic cavity, including the heart, breast, or even the brain.
Deep infiltrating endometriosis is a rare condition that is not easy to diagnose.
How Is Deep Infiltrating Endometriosis Diagnosed?
It can be challenging to diagnose deep endometriosis promptly.
However, advanced diagnostic tools can help doctors accurately diagnose and locate even the most advanced cases of deep infiltrating endometriosis.
Steps of deep endometriosis diagnosis include:
- Check for endometriosis symptoms: Most patients with endometriosis complain of pelvic pain, dysuria (pain when urinating), dysmenorrhea (painful menstrual periods), dyspareunia (pain associated with sex), digestive discomfort, and rectal bleeding.
- Physical examination: During a physical exam, the uterus, ovaries, vaginal fornix, rectovaginal septum, vesicouterine septum, and parametrium are checked.
- Imaging tests: Advanced imaging techniques help create images of your reproductive organs and localize deep infiltrating endometriosis.
The advanced imaging tools in use at prominent centers include:
- 2D/3D vaginal and Introital Ultrasound: This is the primary imaging exam. It helps visualize the endometrium and the surrounding pelvic area. It also helps determine how far endometriosis has advanced.
- Abdomino-pelvic MRI: This diagnostic imaging test helps to learn extra details, such as the localization of the lesions, the presence of extra-pelvic nodes, and whether there is any urinary involvement.
Depending on technological capabilities and the experience and expertise of the care team, patients may receive adequate medical and surgical advice after only an endometriosis ultrasound without needing further exams.
What Are The Challenges Of Managing Deep Infiltrating Endometriosis?
Deep infiltrating endometriosis is the most aggressive type of endometriosis. Therefore, choosing the best therapeutic approach for women with deep endometriosis can be challenging.
The management of this condition will depend on the endometriosis stage, the severity of symptoms, the patient’s medical history, and the patient’s personal choice.
Some of the challenges faced during the management of deep infiltrating endometriosis include:
- Difficulty evaluating the severity of the condition and planning the adequate steps to manage it
- An inaccurate diagnosis can lead to unnecessary or ineffective surgeries
- The management of deep endometriosis requires a multidisciplinary team inside and outside the operating room
A collaborative approach helps to plan the best and safest treatment options for endometriosis before proceeding to surgery. This helps to:
- Avoid surprises and unexpected findings during the surgery
- Succeed in managing the symptoms of endometriosis
- Lower the complication rate from surgery
- Improve fertility
What Are The Advancements in Managing Deep Infiltrating Endometriosis?
Surgery for endometriosis is proposed only in the following cases:
- If the patient has pain associated with endometriosis
- The patient did not respond to medical treatment (such as hormone therapy)
- The patient cannot receive hormone therapy
- The patient has a good ovarian reserve (number of healthy eggs in the ovaries)
- The patient has infertility concerns
Developments in minimally invasive surgical techniques can help avoid post-op complications and preserve fertility.
Below are some new technologies and advancements used to treat endometriosis.
PlasmaJet surgical device
Ovarian cystectomy is a minimally invasive surgery that removes endometriosis cysts from the ovaries. This laparoscopy for endometriosis is recommended only for women with healthy eggs in the ovaries.
Women with low ovarian reserve could not receive ovarian cystectomy to manage endometriosis. Studies have shown that ovarian tissue damage caused by the surgical procedure can harm the remaining follicles and affect ovarian reserve.
To resolve this challenge, surgeons switched to PlasmaJet, a new endometriosis treatment strategy. The PlasmaJet is a surgical device that allows surgeons to treat ovarian cysts without damaging the surrounding ovarian tissue.
This helps protect the low ovarian reserve and increases the possibility of pregnancy after endometriosis surgery.
Indocyanine green (ICG) fluorescence
Another challenge surgeons face during endometriosis surgery is minimizing the amount of dissected tissue.
During laparoscopy for endometriosis, surgeons aim to remove the maximum amount of infiltrating endometrial tissue without damaging the surrounding healthy tissue.
Indocyanine green (ICG) fluorescence imaging is one of the recent developments in video imaging during surgery. ICG technology involves injecting a green dye in the Ureter during a cystoscopy.
The fluorescent green dye allows surgeons to visualize the details of the uterus and safely remove the maximum amount of infiltrating endometrial tissue without damaging the urinary tract.
This new technology helps avoid unnecessary tissue removal and decreases the risk of needing another surgery.
Stenting during partial cystectomy
The bladder is one of the most affected areas in urinary endometriosis. Therefore, the surgical treatment of urinary endometriosis often involves partial cystectomy (partial bladder removal).
Ureteral stenting during bladder surgery is one of the required techniques to protect the ureters (tubes through which urine travels from the kidneys to the bladder) from further damage.
Surgeons can place stents in a minimally invasive manner during the bladder surgery itself without the need for further surgery. That helps protect the ureters and decrease the risk of urinary complications after bladder endometriosis surgery.
Endometriosis and Fertility
Fertility is a common concern among women with endometriosis. Most women want to ensure they can still get pregnant after endometriosis treatment or surgery.
Therefore, surgeons employ atraumatic surgical techniques to avoid injuring delicate structures in the reproductive system and improve the chances of pregnancy.
Doctors typically include the patient in the decision-making while weighing the risks and benefits of surgery.
When a patient with deep infiltrating endometriosis seeks IVF, endometriosis experts coordinate with IVF experts to ensure the best possible clinical outcome.
Deep infiltrating endometriosis is often a complex and challenging condition that can compromise fertility. However, with the most advanced endometriosis treatment options, managing pain associated with this condition and preserving fertility is possible.

Dr. Pedro Barri Soldevila is a Gynecological Surgeon and the Head of the Department of Obstetrics, Gynecology and Reproductive Medicine at Dexeus University Hospital (Quironsalud) in Barcelona, Spain. His main areas of interest include Deep Infiltrating Endometriosis, Pelvic Floor and Reproductive surgery.
Dr. Barri has been part of the Board of Directors of AAGL, representing Europe, Middle East and Africa. He has also done an Executive Program at Harvard Business School on Management in Healthcare Delivery, as well as participated in many humanitarian surgical trips to Africa.
He has also received an Award: IMPULSA 2011 for FGM Reconstruction Program by His Majesty King Felipe VI, Honorary President of FPdGI Foundation.

The Deep Endometriosis unit at Dexeus University Hospital (Quironsalud) in Barcelona is one of the largest in Spain and Europe. The unit has a multidisciplinary team of medical professionals, including ultrasound experts, fertility specialists, gynecologists, and surgeons. The surgeons at Quironsalud Dexeus Hospital are extensively trained in deep infiltrating endometriosis surgery and pelvic floor laparoscopy, enabling them to perform the safest and most effective surgical procedures.
The Endometriosis Unit receives many patients who have been previously operated on, which makes cases more challenging. On average the unit receives 2,000 patients annually, with almost 1,000 endometriosis operations performed. The interdisciplinary collaborative approach minimizes unexpected findings in the OR, seen in less than 1%
Sources:
Featured Blogs



