Treatment for Barrett’s Esophagus
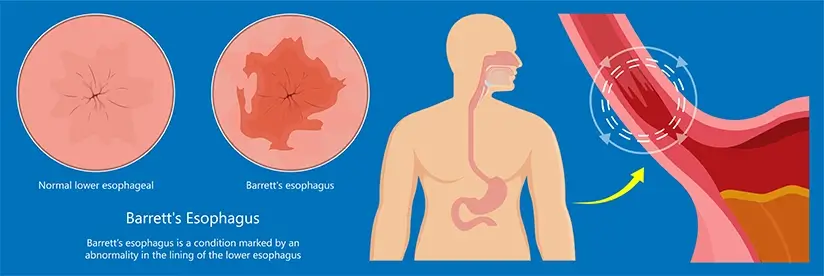
Barrett’s Esophagus is a condition that affects the lower part of the esophagus - the muscular tube which transports food from your mouth to your stomach.
It’s usually associated with acid reflux disease (GERD) - a very common condition with worldwide prevalence rates ranging from 8-40%. The continuous exposure to stomach acid causes the esophageal cells to change, and they start to resemble intestinal cells. This change can sometimes lead to cancer of the esophagus. This is why early diagnosis and management are critical. Studies indicate an incidence of 1.3 to 1.6% among the general population for Barrett’s Esophagus and that 5 to 15% of symptomatic GERD patients are at risk of Barrett’s Esophagus. It impacts males more (3:1) and is more common in those of white ethnicity, with incidence increasing with age. Furthermore, obesity (with high abdominal fat rather than BMI) is another prominent risk factor for both conditions.
Diagnosis is done through endoscopy and biopsies. Treatment involves lifestyle changes, endoscopic resection, radiofrequency ablation, and acid-suppressing medications.
Leading gastroenterology centers utilize the most innovative diagnostic and therapeutic techniques to effectively treat Barrett’s esophagus, focusing on eradicating abnormal cells and reducing recurrence rates with minimal risks.
What Is Barrett’s Esophagus?
Barrett’s Esophagus is a pathologic condition of the esophagus. It’s thought to be a complication of gastroesophageal reflux disease (GERD), however, it can occur without it.
The condition occurs in the lower part of the esophagus, called the “lower esophageal sphincter” or LES. This is the part of the esophagus directly before the stomach, and at the greatest risk of being damaged by stomach acid.
Barrett’s Esophagus occurs when the cells lining the wall of the lower esophagus (LES) change their type. They start to resemble intestinal cells and grossly appear as distinctive pink lesions in the lower esophagus.
Although rare, Barrett’s Esophagus can sometimes lead to esophageal cancer. Doctors classify Barrett’s Esophagus as a precancerous lesion and treat it aggressively.
Symptoms of Barrett’s Esophagus
Most of the time, Barrett’s Esophagus is associated with stomach acid reflux. As such, the symptoms of Barrett’s Esophagus can include:
- Recurring and long-standing heartburn
- Difficulty swallowing food
- Frequent regurgitation
- Upper belly burning pain
These symptoms are not specific to Barrett’s Esophagus and are rather common symptoms of GERD. The chronic nature of these complaints may prompt your doctor to rule out Barrett’s Esophagus using endoscopy.
Keep in mind that Barrett’s Esophagus can occur even without having gastric acid reflux. In such cases, the symptoms of reflux are minimal.
Diagnosis of Barrett’s Esophagus
Early diagnosis of Barrett’s Esophagus is essential to treat the condition and reduce the risk of esophageal cancer. Barrett’s Esophagus is diagnosed using:
- Upper Endoscopy: Also called Gastroscopy, it’s the main tool to diagnose Barrett’s Esophagus. Endoscopy involves the use of an endoscope - a flexible cord-like device with a camera and a light source at its tip. The endoscope is inserted through the mouth and advanced into the esophagus until it reaches the stomach. Your gastroenterologist will see the inside of the esophagus in real-time on a screen. Abnormal pink and eroded lesions of the lower esophagus raise suspicion of Barrett’s Esophagus.
- Biopsies: During gastroscopy, your doctor will take tissue samples (biopsies) from any suspicious lesions. These will be carefully studied by pathologists to determine whether you have Barrett’s Esophagus or not.
Today, top gastroscopy centers can accurately detect even the smallest abnormal lesions during endoscopy using advanced technologies.
Diagnostic Findings
Based on the result of the biopsy, your pathologist will determine the amount of “dysplasia” you have.
Dysplasia is an advanced cellular change that can occur within a Barrett’s Esophagus lesion. The more dysplasia you have, the more significantly mutated the cells are. Dysplasia is considered a precancerous lesion.
So, your pathologist will classify the lesion you have as Barrett’s esophagus with:
- No dysplasia: You have Barrett’s Esophagus, but no dysplastic cells
- Low-grade dysplasia: You have Barrett’s Esophagus with cells showing some abnormalities
- High-grade dysplasia: You have Barrett’s Esophagus with cells showing significant abnormalities. These are cells possibly on the way to becoming cancerous cells.
- Early Barrett´s cancer: You have Barrett’s Esophagus with cells showing cancerous cells.
What is the best Treatment for Barrett’s Esophagus
The treatment of Barrett’s esophagus depends on the degree of dysplasia found on the biopsy:
No Dysplasia
If your biopsy shows no dysplastic cells, then the likelihood of developing cancer is extremely low. As such, a more conservative treatment strategy that involves could be followed:
- Lifestyle changes: Lifestyle changes, such as dieting, doing sports, and organizing mealtimes would be recommended. These aim to reduce acid reflux and allow the esophagus to heal.
- Acid-suppressive medications: You will be prescribed some medications to reduce acid production by the stomach (e.g. Proton Pump Inhibitors - PPIs)
- Follow-up endoscopies: Having no dysplasia does not mean there’s no risk of cancer. This is why gastroscopy needs to be repeated periodically to monitor for any new changes. The first gastroscopy is done 1 year after the initial diagnosis. If no dysplasia is found, a gastroscopy is recommended every 3 to 5 years afterward.
Low-grade Dysplasia
If you have low-grade dysplasia, then you’re at a slightly higher risk of developing cancer in the future.
Depending on your other risk factors, your doctor might either recommend aggressive monitoring (endoscopy every 6 to 12 months) or treatment of the lesion. If treatment is recommended, your options include:
- Surveillance: Follow-up endoscopies with biopsies (see above)
- Cryotherapy: Another method to treat Barrett’s esophagus involves the use of extreme cold. A freezing liquid (e.g. nitrogen) is injected into the lesions to destroy abnormal cells.
- Radiofrequency ablation: Using the endoscope, radio waves can be used to bombard the lesions with high energy. These will effectively destroy abnormal cells.
Major global centers perform the most advanced therapeutic interventions to treat Barrett’s esophagus, maintaining strict treatment protocols and follow-up regimens to ensure that all precancerous cells are destroyed to reduce the risk of recurrence.
High-grade Dysplasia or early Barrett´s Carcinoma
If your pathology report shows high-grade dysplasia, then you’re at a higher-than-usual risk of developing esophageal cancer.
In such cases, monitoring alone is not an option. Treatment of Barrett’s esophagus with high-grade dysplasia or early Barrett´s carcinoma includes:
- Endoscopic submucosal resection or endoscopic mucosal resection Your gastroenterologist will cut out the lesions using endoscopy. With the guidance of the gastroscope’s camera, your doctor will identify the lesions. He or she will then scrape the inner layer of the esophagus using endoscopic scissors to remove the dysplastic cells. This is one of the most advanced minimally-invasive ways to treat Barrett’s esophagus without open surgery
- Cryotherapy (explained above)
- Radiofrequency ablation (explained above)
- Esophagectomy: In some cases, surgical resection of the diseased part of the esophagus might be needed to prevent progression to cancer. This is usually performed by a thoracic or visceral surgeon.
After removing the lesion, a close monitoring plan and periodic gastroscopy examinations are recommended, usually yearly.
Early diagnosis and treatment of Barrett’s esophagus is the key to achieving remission and preventing progression to cancer.

Prof. Dr. med. Siegbert Faiss is the Head of Department for Internal Medicine, with a focus on gastroenterology at the Sana Hospital Lichtenberg. Being a nationally and internationally recognized gastroenterologist and interventional endoscopist, he has received numerous honors and prizes for his scientific work, especially in the field of endosonography and endoscopic tumor therapy.
Acclaimed and awarded for exceptional quality in gastroenterological care, the Department for Internal Medicine is a hub of ongoing innovative research on the Barrett’s Esophagus condition. As such, we implement the latest and most well-studied therapeutic and diagnostic techniques science has to offer.
For more details on the Doctor, visit this link.
To explore the entire scope of services offered by the Department for Internal Medicine, with a focus on gastroenterology at the Sana Hospital Lichtenberg, visit here.
Sources:
Featured Blogs



