Types of Corneal Surgery: From Transplants to Cross-Linking
Types of Corneal Surgery:
Corneal Transplant (Keratoplasty) -
Photorefractive Keratectomy (PRK) -
LASIK (Laser-Assisted in Situ Keratomileusis) and Femto-LASIK
Phototherapeutic Keratectomy (PTK) -
Superficial Keratectomy (SK) -
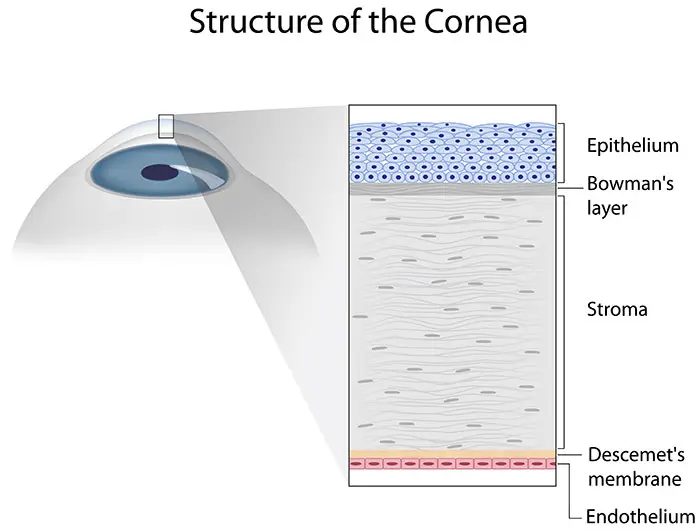
The cornea is essential for clear vision, functioning as the eye's outermost lens to focus light onto the retina. It comprises five distinct layers: the epithelium, Bowman's layer, stroma, Descemet's membrane, and endothelium. These individual layers play a crucial part in ensuring corneal transparency, which is vital for overall eye health.
Corneal surgery encompasses various procedures aimed at repairing or replacing the cornea to restore or enhance vision. These surgeries address issues such as corneal scarring, thinning, swelling, and degenerative conditions, ultimately improving vision, reducing pain, and preventing further corneal deterioration.
Corneal conditions are one of the leading causes of vision impairment globally. Although their prevalence varies by region, advancements in corneal surgery have provided effective treatments, significantly enhancing the quality of life for many people.
Corneal Disease
Causes
Corneal diseases can arise from various causes, including genetic factors, infections, injuries, and degenerative conditions. Some common causes include:
- Keratoconus: Where the cornea, the clear dome at the front of the eye, progressively thins and bulges outward.
- Fuchs' Dystrophy: A genetic disorder leading to the gradual deterioration of the corneal endothelium.
- Infections: The cornea is susceptible to ulcers and scarring from infections caused by bacteria, viruses, or fungi.
- Trauma: Physical injuries or chemical burns can damage the cornea.
Common Symptoms
Symptoms of corneal disease can vary but often include:
- Blurred or distorted vision
- Eye pain or discomfort
- Sensitivity to light (photophobia)
- Redness or inflammation of the eye
- Excessive tearing or discharge
- A feeling of a foreign object in the eye
When is Surgery Necessary?
Surgery may be necessary when corneal disease significantly impairs vision or causes chronic pain that cannot be managed with non-surgical treatments. Indications for corneal surgery include:
- Advanced keratoconus not responding to other treatments
- Severe corneal scarring from infections or injuries
- Progressive thinning or swelling of the cornea
- Conditions like Fuchs' dystrophy that do not respond to medical therapy
In such cases, surgical interventions, such as corneal transplants, cross-linking, or other procedures, may be recommended to restore vision and improve quality of life.
Types of Corneal Surgery
Corneal Transplant (Keratoplasty)
Penetrating Keratoplasty (PK)
Penetrating Keratoplasty (PK) is a full-thickness corneal transplant. The damaged or diseased cornea is entirely removed, and a healthy donor cornea is sutured in place.
PK is used for severe corneal diseases such as advanced keratoconus, deep corneal scarring, and severe corneal dystrophies. Candidates include patients with significant vision loss or pain due to corneal damage. Contraindications include active infections and conditions affecting the integrity of the eye.
Side Effects and Considerations
Infection, graft rejection, and astigmatism are some possible side effects. Considerations involve the need for lifelong anti-rejection eye drops and a potentially prolonged recovery period.
Recovery Process and Post-Operative Care
Recovery can take several months to a year. Successful treatment relies on adhering to the drug regimen prescribed and follow-up appointments to monitor for graft rejection and other complications.
Success Rates and Long-Term Outcomes
Success rates are generally high, with long-term graft survival rates improving over the years. However, there is a risk of graft rejection, and some patients may require additional procedures.
Lamellar Keratoplasty
Lamellar Keratoplasty involves replacing only the affected layers of the cornea, preserving the healthy layers. This includes Deep Anterior Lamellar Keratoplasty (DALK) and Endothelial Keratoplasty procedures like Descemet's Membrane Endothelial Keratoplasty (DMEK) and Descemet's Stripping Automated Endothelial Keratoplasty (DSAEK).
Deep Anterior Lamellar Keratoplasty (DALK)
DALK involves removing the front layers of the cornea down to the Descemet's membrane and replacing them with donor tissue.
DALK is indicated for conditions affecting the corneal stroma, such as keratoconus and superficial scars. Patients who might not be suitable for full-thickness transplants and those who have healthy endothelium are candidates for this surgery.
Side Effects and Considerations
Side effects may include interface haze and incomplete removal of the diseased stroma. The procedure is technically challenging, which might necessitate converting it to PK if complications arise.
Recovery Process and Post-Operative Care
Recovery is generally faster than in cases of PK, with fewer risks of rejection since the endothelium remains intact. Post-operative care includes regular monitoring and medication to prevent infection and inflammation.
Success Rates and Long-Term Outcomes
DALK has a high success rate and fewer complications than PK. Long-term outcomes are positive, with a reduced risk of endothelial rejection.
Descemet's Membrane Endothelial Keratoplasty (DMEK)
DMEK involves replacing only the diseased endothelial layer and Descemet's membrane with donor tissue.
DMEK is indicated for endothelial disorders like Fuchs' dystrophy and pseudophakic bullous keratopathy. Patients with endothelial dysfunction but healthy anterior corneal layers are candidates for this surgery.
Side Effects and Considerations
Side effects may include graft dislocation and primary graft failure. Besides, the precision involved requires a high degree of surgical skill and careful handling of delicate tissue.
Recovery Process and Post-Operative Care
Recovery is typically quicker with DMEK, and visual outcomes are often excellent. Patients need to follow strict post-operative care instructions to ensure graft adhesion and prevent complications.
Success Rates and Long-Term Outcomes
DMEK has a high success rate and excellent long-term outcomes, with lower rejection rates compared to PK and DSAEK.
Descemet's Stripping Automated Endothelial Keratoplasty (DSAEK)
DSAEK involves replacing the endothelium and part of the stroma with donor tissue using an automated system.
DSAEK is used for endothelial dysfunctions similar to DMEK, such as Fuchs' dystrophy and corneal edema. Patients with endothelial failure who cannot undergo DMEK due to anatomical or technical reasons are candidates for this procedure.
Side Effects and Considerations
Side effects may include graft detachment and interface haze. Considerations involve the surgical technique and the need for precise tissue preparation.
Recovery Process and Post-Operative Care
Recovery is generally good, though slightly longer than DMEK. Post-operative care focuses on preventing graft dislocation and managing inflammation.
Success Rates and Long-Term Outcomes
DSAEK has a high success rate, good visual outcomes, and a reduced risk of rejection compared to PK. Long-term outcomes are favorable, though DMEK may offer superior visual acuity in some cases.
Both DMEK and DSAEK are types of Endothelial Keratoplasty, each with specific indications, benefits, and considerations. The optimal approach depends on the patient's condition, the surgeon's skills, and other individual factors.
Keratoprosthesis (KPro)
Keratoprosthesis involves the implantation of an artificial cornea when traditional corneal transplants fail or are not feasible. The most common type is the Boston Keratoprosthesis.
KPro is used for severe corneal opacities, multiple failed corneal transplants, and conditions like Stevens-Johnson syndrome. Candidates are typically those who have no other surgical options for vision restoration.
Side Effects and Considerations
Potential complications include infection, glaucoma, and retinal detachment. Long-term use of antibiotics and anti-inflammatory medications is necessary to prevent complications.
Recovery Process and Post-Operative Care
Recovery involves close monitoring and adherence to medication regimens. Regular follow-ups are crucial to manage potential complications.
Success Rates and Long-Term Outcomes
Success rates are high for vision improvement, but long-term management is essential due to the risk of complications.
Refractive Surgery
Photorefractive Keratectomy (PRK)
Photorefractive Keratectomy (PRK) utilizes an excimer laser to ablate the corneal epithelium and reshape the corneal stroma to correct refractive errors.
PRK is used for myopia, hyperopia, and astigmatism in patients with thinner corneas or those who participate in contact sports where flap complications from LASIK might be a concern.
Side Effects and Considerations
Side effects may include discomfort, haze formation, and longer recovery time due to the removal of the epithelium, which requires time to heal.
Recovery Process and Post-Operative Care
Recovery takes several weeks for the vision to stabilize. Post-operative care includes using anti-inflammatory and antibiotic eye drops.
Success Rates and Long-Term Outcomes
PRK has high success rates and excellent long-term outcomes. Vision correction is stable once healing is complete.
LASIK (Laser-Assisted in Situ Keratomileusis) and Femto-LASIK
LASIK and Femto-LASIK involve creating a corneal flap, sculpting the corneal tissue with a laser, and repositioning the flap to correct vision. The difference between LASIK and Femto-LASIK is that the cut to create the corneal flap is performed with a mechanical microkeratome in LASIK, while in Femto-LASIK, it is performed with a Femtosecond laser, which is much more precise and less traumatic for the eye.
LASIK and Femto-LASIK are used for myopia, hyperopia, and astigmatism. Eligible candidates must have adequate corneal thickness and stable refractive errors.
Side Effects and Considerations
Side effects may include dry eyes, glare, and potential flap complications. Corneal thickness is crucial for ensuring enough tissue remains post-surgery.
LASIK and Femto-LASIK offer quicker recovery and less discomfort but carry risks related to the flap. PRK is safer for those with thinner corneas or at a higher risk of trauma.
Recovery Process and Post-Operative Care
Recovery is typically faster compared to PRK, with most patients achieving good vision within days. Post-operative care includes using prescribed eye drops and protecting the eyes from trauma.
Success Rates and Long-Term Outcomes
LASIK and Femto-LASIK have high success rates and excellent long-term outcomes. Advanced techniques like Wavefront-Guided LASIK can enhance visual quality and reduce complications.
Phototherapeutic Keratectomy (PTK)
PTK uses an excimer laser to remove superficial corneal tissue, treating conditions like scars, dystrophies, and recurrent erosions.
PTK is indicated for superficial corneal diseases and scarring. Candidates are those with non-infectious superficial corneal conditions.
Side Effects and Considerations
Side effects include haze and prolonged healing. It is vital to ensure the underlying cause of the corneal issue is addressed. Mitomycin C is currently used to reduce side effects and improve results.
Recovery Process and Post-Operative Care
Recovery involves the regrowth of the epithelium, taking a few weeks. Post-operative care includes medications to prevent infection and promote healing.
Success Rates and Long-Term Outcomes
PTK has high success rates for treating superficial corneal issues, with long-term outcomes generally favorable.
Pterygium Surgery
In this procedure, the pterygium, a benign growth on the cornea, is removed, followed by conjunctival autografting or amniotic membrane transplantation to reduce recurrence.
Surgery is indicated for symptomatic pterygium causing irritation, vision impairment, or cosmetic concerns. Candidates are those with progressive or large pterygium.
Side Effects and Considerations
Side effects include recurrence, infection, and scarring. Considerations involve the technique used to minimize recurrence rates.
Recovery Process and Post-Operative Care
Recovery involves managing inflammation and promoting healing with medications. Follow-up is essential to monitor for recurrence.
Success Rates and Long-Term Outcomes
Success rates are high with appropriate surgical techniques. Long-term outcomes are favorable, with a low recurrence rate using advanced methods.
Superficial Keratectomy (SK)
Superficial Keratectomy involves the removal of the superficial corneal layer to treat conditions like band keratopathy, corneal dystrophies, and recurrent erosions.
SK is indicated for superficial corneal deposits and irregularities in patients with non-responsive or recurrent conditions.
Side Effects and Considerations
Side effects include discomfort and haze. Considerations involve the underlying condition and ensuring thorough removal of abnormal tissue.
Recovery Process and Post-Operative Care
Recovery involves re-epithelialization of the cornea, taking several weeks. Post-operative care includes using eye drops to manage pain and prevent infection.
Success Rates and Long-Term Outcomes
SK has high success rates for removing superficial corneal irregularities. Long-term outcomes are positive with proper management.
Intrastromal Corneal Ring Segments (ICRS)
ICRS involves inserting crescent-shaped rings into the corneal stroma to flatten the cornea and correct refractive errors like keratoconus.
ICRS is indicated for keratoconus and ectatic disorders. Candidates are those with mild to moderate keratoconus unsuitable for cross-linking alone.
Side Effects and Considerations
Side effects include infection, ring migration, and glare. Considerations involve careful patient selection and precise placement of the rings.
Recovery Process and Post-Operative Care
Recovery involves several weeks of healing. Post-operative care includes managing inflammation and ensuring ring stability.
Success Rates and Long-Term Outcomes
ICRS has moderate to high success rates for improving vision and stabilizing keratoconus. Long-term outcomes are generally positive with appropriate follow-up.
Corneal Cross-Linking
Corneal Cross-Linking (CXL) strengthens the cornea by applying riboflavin (vitamin B2) and exposing it to ultraviolet light, forming new cross-links between collagen fibers.
CXL is primarily used for keratoconus and ectasia after LASIK. Those with progressive keratoconus and suitable corneal thickness are candidates for this procedure.
Side Effects and Considerations
Side effects include discomfort, haze, and risk of infection. Considerations include ensuring adequate corneal thickness and the absence of scarring or severe haze.
Recovery Process and Post-Operative Care
Epithelial healing happens over a few days to weeks. Post-operative care includes using antibiotics and anti-inflammatory medications.
Success Rates and Long-Term Outcomes
CXL has high success rates in halting the progression of keratoconus. Long-term outcomes are positive, with many patients experiencing stabilization and, in some cases, improved corneal shape.
Latest News and Advancements in Corneal Surgery
Recent advancements in corneal surgery have significantly improved patient outcomes and expanded treatment options. Personalized treatments, including customized transplants and laser-assisted surgeries, offer precise interventions tailored to individual patient needs.
Advanced tissue engineering has led to the development of bioengineered corneas, presenting a significant solution to the limitations of donor cornea availability. These corneas exhibit excellent biocompatibility, integrating well with the host tissue. Additionally, functional outcomes achieved with bioengineered corneas are comparable to those observed with traditional corneal grafts.
Gene therapy offers a new frontier for treating genetic corneal disorders by targeting and correcting specific genetic mutations, potentially halting or reversing disease progression without repeated surgeries.
Technological innovations are also transforming corneal surgery. Femtosecond Laser-Assisted Keratoplasty (FLAK) enhances graft placement accuracy and visual outcomes. Limbal Stem Cell Transplant (LSCT) promotes corneal healing by replacing and restoring the function of damaged or missing limbal stem cells in patients with limbal stem cell deficiency. Artificial intelligence (AI) and robotic surgery improve diagnostic precision, predict surgical outcomes, and offer greater precision for intricate surgeries, minimizing errors and improving success rates.

Dr. Carlos Vergés Roger is the Head of Ophthalmology at Dexeus University Hospital (Quirónsalud). Specialized in Advanced Ophthalmology, Dr. Vergés and his team deliver cutting-edge technological, medical, and surgical expertise. After graduating in Medicine and Surgery from the Faculty of Medicine of the University of Barcelona, Dr. Vergés moved to Boston (USA) to pursue research in ophthalmology, completing a doctorate in Biology from Harvard University. His areas of interest focus on cornea, cataracts, and the neurophysiological mechanisms of vision, especially those related to sports.

Dexeus University Hospital (Quirónsalud), also known as the 'Knowledge Hospital', is the center of reference in many of its specialties, being one of the first private university centers in all of Spain. The hospital has a solid team of more than 450 medical professionals and incorporates the latest functional and technological advances typical of leading centers. Every year, 49,000 hospital stays are registered, more than 85,000 emergencies are treated (about 230 daily), 10,000 plus surgical interventions are performed, and over 2,500 deliveries and around 50 clinical trials are carried out at the hospital. The Ophthalmological Institute at Dexeus University Hospital specializes in various fields of ophthalmology, utilizing the most modern technological equipment and advanced diagnostics. The team delivers comprehensive medical care and the most advanced surgical treatments for eye health. In addition, as vision problems are closely related to general health, they collaborate closely with medical specialties such as internal medicine, endocrinology and nutrition, rheumatology, gynecology, and others to offer comprehensive treatment.
References:
Featured Blogs



