All You Need to Know About Dyshidrosis
Originally Authored by Dr. Lauren Livelo - April 14, 2022
Medically Reviewed and Updated by Dr. Sony Sherpa, (MBBS) - July 05, 2024
What is Dyshidrosis?
Dyshidrosis, or otherwise known as Dyshidrotic eczema, is a chronic skin condition that appears as small, itchy blisters on the feet and hands, more common on the lateral sides of fingers and toes. It is common in young adults between the ages of 20 and 40 and is more frequent in women than men. Some cases resolve quickly, but others can persist for long periods.
Causes of Dyshidrosis
The exact cause for dyshidrotic eczema has not yet been identified, but it is hypothesized to have a genetic component. There are a variety of triggers causing the appearance of these lesions. Risk factors include:
- Having another type of eczema, such as atopic dermatitis
- Personal / family history of asthma, allergic rhinitis (hay fever), eczema
- Nickel or cobalt allergies
- Medications (aspirin, birth control pills)
- Irritants or allergies to ingredients in the skincare products used
- Sweaty hands and/or feet
- Exposure to a lot of wet work such as washing dishes, laundry
- Occupations related to metalwork, mechanics
- Changes in weather
- Hot temperatures
- Stress
Dyshidrotic eczema is not contagious. Flare-ups are often triggered by exposure to nickel, a very common metal. Stressful events and changes in weather are also typical triggers.
Symptoms
Dyshidrotic eczema appears as deep-seated blisters, or what we call vesicles, on the hands and feet. It is most commonly found on the sides of your fingers and toes but can also appear on the palms. Some vesicles group together to form larger blisters. It can be accompanied by intense itching and sometimes, a burning or prickly sensation. Scratching these itchy vesicles can create breaks in the skin and cause secondary bacterial infections with some swelling, redness, and crusting of the lesions.
Dyshidrotic eczema improves in a few weeks. As the blisters clear out, they can leave dark marks (post-inflammatory hyperpigmentation) on the skin. The skin can also appear to be dry and scaly.
Diagnosis
Diagnosing dyshidrotic eczema typically involves a clinical examination and patient history. Specific tests confirm your diagnosis and exclude other possibilities:
- Allergy testing, such as a patch test, may be used to identify potential triggers.
- The presence of dyshidrotic eczema is confirmed through the appearance of characteristic vesicles on the hands and feet.
- Skin biopsy and blood tests can be conducted to rule out infections or other types of eczema.
- A potassium hydroxide (KOH) test may be performed to exclude fungal infections.
- Identifying the exact cause and triggers through these tests helps in tailoring the treatment plan to the individual's specific needs.
Similar Diseases
Several conditions can mimic dyshidrotic eczema, making diagnosis challenging:
- Pompholyx eczema (vesicular eczema): Presents similarly with itchy blisters but typically affects the palms and soles.
- Palmoplantar pustulosis: Involves pustules rather than clear vesicles and can also cause scaling and thickening of the skin.
- Other conditions: Allergic contact dermatitis, tinea manuum (fungal infection), and pustular psoriasis.
Different conditions require different treatments, so an accurate diagnosis ensures you get the best care. A thorough examination and detailed medical history are essential to distinguish between these similar diseases.
Complications
- Scarring from chronic scratching and popping blisters should be avoided to prevent infections and further skin damage.
- Persistent scratching can lead to lichenification, where the skin becomes thick and leathery.
- Eczema herpeticum: A severe complication caused by herpes simplex virus infection, characterized by painful, rapidly spreading blisters, requiring immediate medical attention.
- Emotional and psychological impacts: Anxiety and depression can arise from the chronic nature of the condition and its visible symptoms.
- Maintaining proper skin care and avoiding known triggers are essential to prevent these complications.
Summer Finger Bumps
Precautions:
- Keep the skin cool and dry.
- Use moisture-wicking gloves and socks.
- Limit time outdoors when it is hot and humid.
- Apply cool compresses and use air conditioning or fans to manage symptoms during the hotter months.
Treatment and Management
There is no cure for dyshidrosis, but there are numerous treatment and management options.
Medications:
- Topical corticosteroids - decrease inflammation and calm the red, inflamed skin
- Topical immunomodulators - keep the immune system from overreacting and producing more inflammation
- Oral antihistamines - address the itch
- Topical or Oral antibiotics - target the secondary bacterial infection, if present
- Topical or Oral antifungals - used if there is a concomitant fungal infection
- Systemic medications such as corticosteroid pills or systemic immunomodulators may be given for severe cases
- Dupilumab - a biologic that may be used in refractory cases
Alternative and Natural Treatments:
Several alternative treatments have been explored for dyshidrotic eczema:
- Homeopathy: Some people use homeopathic remedies to alleviate symptoms, though scientific evidence is limited.
- St. John’s wort: Applied topically, the anti-inflammatory and wound-healing properties of creams and oils containing St. John’s wort offers relief.
- Dandelion juice: Dandelion is believed to have detoxifying effects and can be consumed as juice or tea.
- Essential oils: Tea tree oil and chamomile are essential oils that, when diluted and used topically, may offer some relief.
It is important to consult with a healthcare provider before trying these treatments to ensure they are safe and effective.
For a comprehensive approach, consider complementary therapies alongside conventional medicine, always under a doctor's guidance.
Procedures:
- Phototherapy – used for moderate cases that are not responsive to initial treatment with topical medications. Phototherapy, which is administered using UV light, helps reduce the inflammatory response of the skin.
- Botulinum toxin injections – decrease hand/feet sweating which can trigger dyshidrosis
Self-care:
- Proper skin care – includes using mild, hypoallergenic, fragrance-free soaps and moisturizers to protect the skin barrier
- Soaks and cool compresses – can help dry blisters
- Remove rings or any jewelry before washing hands
- Avoid scratching
- Manage stress
- Avoid allergens or irritants that trigger your skin
- Wear gloves. Use cotton gloves if your hands will stay dry throughout the day during work. When doing wet work, use cotton gloves under waterproof gloves or rubber gloves.
Prevention and Home Remedies
Preventive measures can help manage dyshidrotic eczema:
- Avoid known triggers such as nickel, which is commonly found in jewelry, zippers, and certain foods.
- Maintain proper hand hygiene by washing hands with mild, hypoallergenic soaps.
- Use emollients regularly to keep the skin moisturized and protect the skin barrier.
- Wear gloves when handling irritants or engaging in wet work, such as dishwashing.
- Home remedies can soothe the skin and reduce itching :
- Oatmeal baths: Add colloidal oatmeal to a lukewarm bath to relieve itching and inflammation.
- Aloe vera gel: Pure aloe vera gel calms and hydrates irritated skin.
- Coconut oil: Use virgin coconut oil as a natural moisturizer with anti-inflammatory properties.
- Cool compresses: Apply cool, damp cloths to the blisters to reduce itching and discomfort.
When to See a Doctor
It is important to consult a healthcare provider if the symptoms of dyshidrotic eczema persist despite over-the-counter treatments or if there are signs of infection, such as:
- Increased redness, swelling, or pus.
- Severe pain or discomfort.
- Blisters that do not improve or worsen over time.
- Any signs of systemic infection, such as fever or chills.
Early intervention prevents complications and improves quality of life with proper treatment.
Diet
Diet can play a role in managing dyshidrotic eczema. While there is no direct link between gluten and dyshidrotic eczema, some people may find relief by avoiding certain foods that trigger flare-ups. Common dietary triggers include dairy, eggs, soy, nuts, and gluten.
Supervised elimination diets uncover food triggers with a doctor's guidance. Dietitians can craft personalized plans to minimize food triggers while ensuring balanced nutrition. Include anti-inflammatory foods like fatty fish, leafy greens, and turmeric to further support healthy skin.
Prognosis
Unfortunately, there is no cure yet for dyshidrotic eczema. Lesions usually improve in about 2-3 weeks, but recurrence is highly possible due to its chronic nature. Triggers such as weather changes, stress, or any exposure to irritants may cause new lesions to appear. Some cases are recalcitrant and will need other forms of treatment to address the skin problem.
Take-Home Messages
Dyshidrotic eczema is a constantly recurring skin disorder that can affect the quality of life of those who have it. It can cause emotional distress and problems with social interactions, which can be a debilitating experience. There are several treatment options for this skin condition; improvements will largely depend on treatment compliance. A visit to the dermatologist is recommended for proper treatment and prompt management. Remember that there is no “magic” treatment and that the rate of improvement differs from person to person.
Frequently Asked Questions
Can Gluten Cause Dyshidrotic Eczema?
While there is no direct evidence linking gluten to dyshidrotic eczema, some people find that their symptoms improve when they avoid gluten. A supervised elimination diet helps pinpoint gluten sensitivity.
Is Dyshidrotic Eczema Linked to Athlete's Foot?
Dyshidrotic eczema and athlete's foot are different conditions, but they can be confused due to similar symptoms. Athlete's foot is a fungal infection, whereas dyshidrotic eczema is a type of eczema. Proper diagnosis is essential for appropriate treatment.
How Common is Dyshidrotic Eczema?
Dyshidrotic eczema affects about 5-20% of people with hand eczema. It is more common in adults aged 20-40 and tends to occur more frequently in women than men.
What is the Fastest Way to Get Rid of Dyshidrotic Eczema?
There is no quick cure, but treatments like high-potency topical corticosteroids, cool compresses, moisturizers, and avoiding triggers can help manage symptoms quickly. Severe cases may require systemic treatments prescribed by a healthcare provider.
How Can I Prevent Dyshidrotic Eczema?
Preventive measures include avoiding known triggers, maintaining proper hand hygiene, using emollients, wearing protective gloves, managing stress, and keeping the skin cool and dry. Regular moisturization and avoiding allergens like nickel can also help reduce flare-ups.
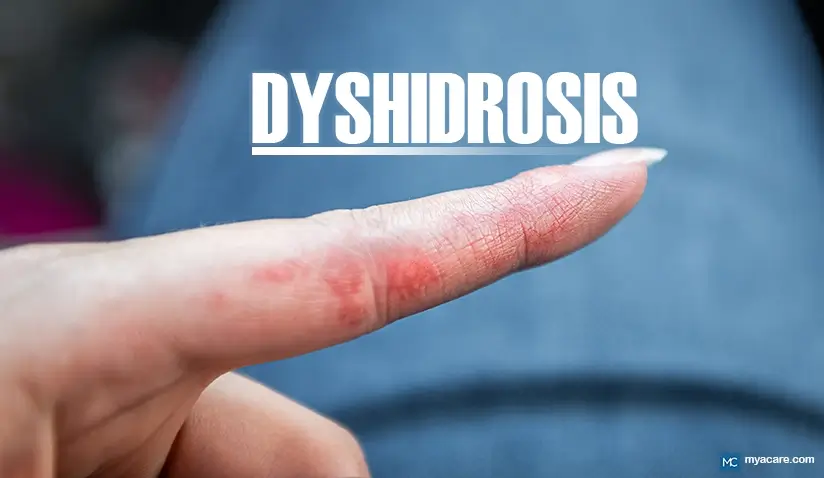
What Does Dyshidrosis Look Like?
Dyshidrosis or dyshidrotic eczema on the hands often appears as small, clear blisters. These blisters typically emerge on the fingers, palms, and the sides of the fingers. They can be quite itchy and are filled with fluid. In some cases, these small bumps cluster together, creating a more pronounced rash that can cause significant discomfort. As the condition progresses, the blisters may dry out and form scales or cracks, particularly if the skin is not properly moisturized.
Dyshidrotic eczema on the feet presents as itchy blisters on the soles and the bottom of the feet and sides of the toe . These blisters are often fluid-filled and can cause considerable itching and discomfort. The affected areas may appear as clusters of small, blistery bumps that can merge to form larger patches. Over time, these blisters may burst and peel, leading to dry, cracked skin. It is common for the condition to flare up periodically, especially in warm or humid conditions.
How Long Does Dyshidrotic Eczema Last?
Dyshidrotic eczema can vary in duration, typically lasting between two to four weeks per episode. The blisters may take about one to two weeks to dry out and heal, leaving behind dry, scaly skin that can persist for another week or more. The frequency and duration of dyshidrotic eczema episodes can vary.
To search for the best health providers for dermatology in Croatia, Germany, Greece, Italy, Malaysia, Singapore, Slovakia Spain, Thailand, The UAE, the UK, and the US, please use our free search engine.
To search for the best healthcare providers worldwide, please use the Mya Care search engine.
The Mya Care Editorial Team comprises medical doctors and qualified professionals with a background in healthcare, dedicated to delivering trustworthy, evidence-based health content.
Our team draws on authoritative sources, including systematic reviews published in top-tier medical journals, the latest academic and professional books by renowned experts, and official guidelines from authoritative global health organizations. This rigorous process ensures every article reflects current medical standards and is regularly updated to include the latest healthcare insights.

Dr. Sony Sherpa completed her MBBS at Guangzhou Medical University, China. She is a resident doctor, researcher, and medical writer who believes in the importance of accessible, quality healthcare for everyone. Her work in the healthcare field is focused on improving the well-being of individuals and communities, ensuring they receive the necessary care and support for a healthy and fulfilling life.
References:
Featured Blogs



