Awake Craniotomy in Brain Surgery: Lessons Learned After 30 Years
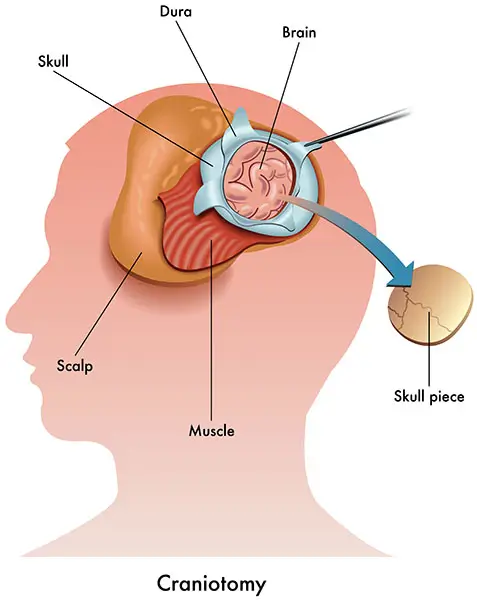
Brain surgery is essential to treat a variety of nervous system conditions. Certain brain conditions, such as an unruptured aneurysm, can usually be treated using minimally invasive, low-risk techniques. However, other brain abnormalities, such as brain tumors, cannot be removed unless the skull is fully opened and the brain is exposed (open brain surgery or craniotomy).
Awake craniotomy is an advanced brain surgery that is conducted while the patient is awake. Over the past 30 years, awake craniotomy has become popular for treating structural problems in the brain while preserving brain functions. By keeping the patient awake, surgeons can map areas of the brain responsible for speech, vision, and movement and avoid them while removing a tumor or an epileptic focus.
What is Awake Craniotomy?
Awake craniotomy, or awake brain surgery, is an open brain surgery that is done while the patient is kept awake using an asleep-awake-asleep technique described in detail below.
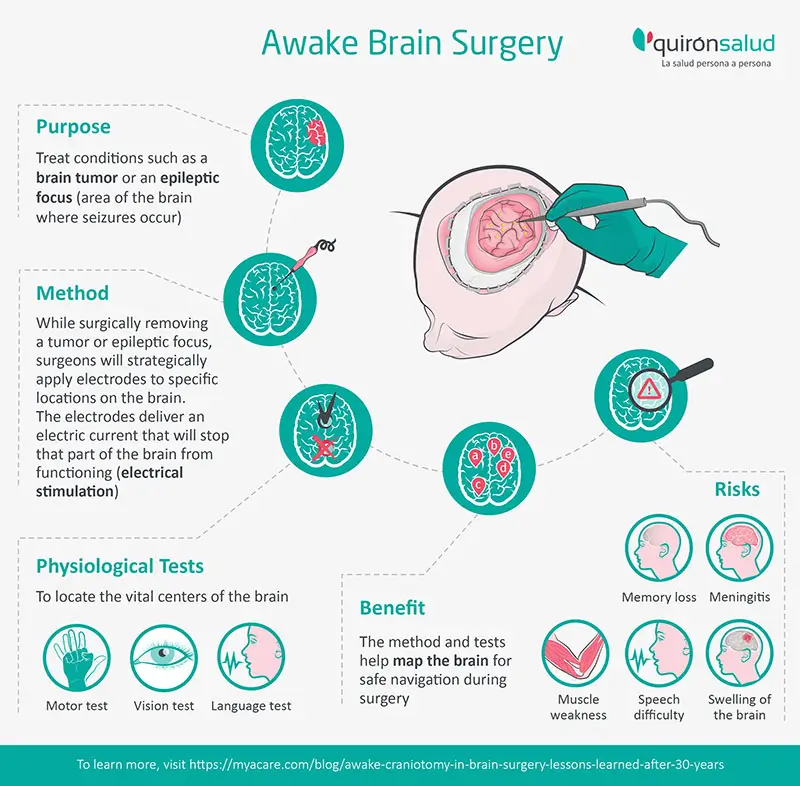
Awake brain surgery is usually performed to treat conditions such as a brain tumor (e.g., glioma) or an epileptic focus (area of the brain where seizures occur).
If the epileptic focus or tumor is close to regions of the brain that govern movement, speech, or vision, the patient may need to be conscious throughout the brain surgery.
During an awake craniotomy, the surgeon performs physiological tests and records the brain's responses. These responses help to accurately treat the area of the brain that needs surgery while avoiding damage to important neurologic functions.
Why is Awake Craniotomy Done?
While surgically removing a tumor or epileptic focus, surgeons need to be sure they don’t damage vital parts of the brain that control your vision, language, or motor skills.
Imaging techniques, including functional MRIs, cannot pinpoint the exact location of these functional brain areas. Awake brain surgery can help locate and avoid the areas of your brain that can affect your movement, eyesight, or speech.
Awake craniotomy, therefore, allows the surgeon to treat the brain and protect its functions by avoiding damaging essential neural pathways.
Positioning of the patient during awake craniotomy
Depending on the part of your brain that needs to be treated during awake cranial surgery, you could be:
- Lying down horizontally on your back (supine position)
- Lying on your side (lateral position)
- In a sitting position (if the tumor is near the vision area of the brain)
Your head will be secured with a headframe and facing the anesthesia team that will carefully monitor your breathing and responses.
How is Awake Craniotomy Done?
Neurosurgeons use an asleep-awake-asleep technique to make the surgery less tiring and more comfortable for the patient. That way, the patient won’t have to be awake for the entire brain surgery:
- First, your head will be secured in a fixed position (usually with a head frame), and you will be put to sleep for the first part of the surgery.
- Then, your surgeon will remove part of your skull to reach your brain.
- After that, the anesthesiologist will stop the sedation to wake you up.
- You will be instructed to perform a task, move a muscle, identify a picture, or answer a question.
- Meanwhile, your surgeon will strategically apply electrodes to specific locations on the brain. The electrodes deliver an electric current that will stop that part of the brain from functioning (electrical stimulation).
- Your responses to the electrical stimulation will be carefully observed. If, for example, you develop movement problems in the arm, this area is marked, and your surgeon will try to avoid it during the resection.
- After doing this several times in different areas of the brain, the surgeon will have a map of the brain centers that control your movement, language, and eyesight.
- The tumor or focus is then cut out while avoiding all those vital centers.
- Finally, the patient will be put to sleep again while the surgeon closes the skull bone and skin wound.
The best neurosurgery centers use advanced intra-operative brain imaging technologies, including 3-D computer imaging and functional MRI, to construct detailed images of your brain.
Neurosurgeons use these images together with brain mapping to guide them safely through the brain during surgery.
What Are the Physiological Tests Done During Awake Craniotomy?
A multidisciplinary team of neurosurgeons, neurologists, neuro-anesthesiologists, and speech-language pathologists will locate the vital centers of the brain during awake surgery using different physiological tests.
Motor tests
If the part of the brain that needs surgery is near your movement center, you will be asked to make certain actions during craniotomy.
When the neurosurgeon delivers electrical stimulation to the brain, a movement may be elicited, for example, closing the hand or moving the foot. This spot of the brain is considered a motor area, and the surgeon marks it specifically. In this way, a complete mapping of the motor areas in the motor strip may be done. The same process is repeated with sensory areas. When current is applied to the brain, the patient feels a sensation similar to tingling in an area of the body. A sensory map of the cortex may thus be elaborated.
The neurosurgeon will avoid those areas as much as possible while cutting out the tumor or epileptic focus.
Language test
Language is a complex function. The regions related to language are usually located around an anatomical structure called the Sylvian Fissure in the brain's dominant hemisphere, usually the left hemisphere. Epilepsy and tumors may reorganize the functional organization of language. This is the most usual indication for an awake craniotomy.
To locate your speech and language centers, a neurosurgeon and a speech-language pathologist will show drawings of common objects (dog, car, window, guitar) and ask the patient to name and describe the drawings, repeat words or sentences, fulfill simple orders, read texts aloud, and perform other tasks. Each of these tests maps specific areas of the cortex that relate to these different sub-functions of language.
Patients that speak different languages may completely overlap the cortical areas or may differ in parts of them. Hence, patients who speak more than one language may be tested in different languages.
Vision test
Mapping your visual tract and centers reduces the risk of partially or completely losing your eyesight while removing tumors or other abnormalities in the visual brain area.
Doctors are trying to develop methods to identify other functions like memory and counting in the future.
What are the Benefits of Awake Craniotomy?
Over the years, neurosurgical advances in awake brain surgery have made it possible to:
- Map and locate functional regions of the brain (responsible for movement, speech, and vision)
- Maximize tumor or epileptic focus removal while preserving neurological function
- Reduce or get rid of epileptic seizures
- Minimize pain after open brain surgery and the need for narcotics
- Reduce the need for postoperative intensive care
- Reduce the risk of neurological complications after surgery
- Improve the survival rate after brain surgery (the less tissue removed, the better the survival rate)
- Adjust the onco-functional balance of the procedure by tailoring the resection
What are the Challenges of Awake Craniotomy?
During the awake phase
The patient may experience:
- Some pain and discomfort. A prepared team of neuro-anesthesiologists will try to keep the patient as comfortable as possible.
- Anxiety and fear: Constant reassurance, encouragement, and conversation from the OR team can help soothe the patient.
- Confusion or agitation: If deep sedation is used in the pre-awake phase, the patient can wake up drowsy and flustered. A sponge soaked with ice-cold water can be used to wet the patient’s lips for comfort.
- Seizures: If the surgeon does not overstimulate the brain areas, seizures are less likely to occur.
- Nausea and vomiting: Avoided by using the right medications.
- Hypertension: Commonly reported during the procedure, hypertension can be managed with appropriate drugs.
After surgery
As with any open brain surgery, after awake craniotomy, there are risks of:
- Memory loss
- Speech difficulty
- Meningitis
- Muscle weakness
- Swelling of the brain
Equipped with innovative technology and extensively experienced medical staff, high-volume centers for awake craniotomy provide patients a detailed neurophysiological assessment before their awake brain surgery to optimize the benefits and reduce challenges during and after the surgery.

Dr. Gerardo Conesa Bertrán is the Chief of Neurosurgery and Director of the Teknon Neuroscience Institute at QS Teknon Medical Center, Barcelona. Dr. Conesa offers extensive expertise in minimally invasive spinal surgery for spinal tumor removal and epilepsy surgery in adults and children. He is also specialized in awake brain surgery of highly functional areas with more than 700 cases performed.
With over 30 years of extensive experience in Neurosurgery, Dr. Conesa has won several awards in recognition of his professional and research career.

Teknon’s neurosurgery center in Barcelona is one of the top brain surgery referral centers in Spain and Europe. Led by Dr. Gerardo Conesa Bertrán, our doctors have vast experience in performing advanced brain imaging and mapping to give their patients the best neurological outcomes from open brain surgery.
Teknon's brain surgery team runs one of the top specialized neurosurgery referral centers in Europe. Our surgeons, neurologists, anesthetists, and therapists have extensive experience in awake brain surgery using the safest and most advanced brain mapping techniques.
For more details, please visit https://www.quironsalud-hospitals.com/
Sources:
Featured Blogs



