Blink and It’s Gone! Vision Loss Types, Causes and Treatment Options
The eyes are a major gateway to the world around us, arguably being the most important out of all the five senses.
In today’s world, this is especially pertinent due to larger volumes of digital work. Eye strain has become a common complaint of the modern era, contributing towards the rising numbers of eye disorders across all age groups. It is estimated that by 2050, just over 1.7 billion people will suffer from some form of visual impairment[1].
The article below describes how the eyes see, when to visit an eye specialist, types of vision disorders, eye treatment options and tips for enhancing the health of the eyes.
How the Eyes See
The eyes consist of a series of parts that work together in order to focus light to a single point, which is then projected onto the retina.[2]
Light passes through the pupil onto the lens, which has a crystalline structure that allows for it to be focused. The aqueous interior of the eyeball provides a perfect environment for this focused light to be projected onto the retina, slowing light down slightly for optimal processing. The retina contains photoreceptive cells (rods and cones) that allow for light to be read and electrochemically processed for the brain to decode via the optic nerve.[3]
The ciliary muscles in the eye are responsible for shaping the lens, accommodating for seeing things at a distance or up close. At rest, the lens is stretched. When in use, the lens relaxes when the ciliary muscles contract in order to make sure the light is refracted optimally. The parasympathetic nervous system plays a role in contracting these muscles, which rounds the lens, constricts the pupils and allows for seeing objects that are close by as well as seeing under intense light conditions. The sympathetic nervous system relaxes the ciliary muscles, resulting in a less rounded lens, dilated pupils, perceiving objects at a distance and vision at low light intensities.
The cones in the eye are responsible for detecting color; while the rods detect contrast, ensuring vision during low-light conditions. When light reaches the retina, the rods and cones absorb it thanks to the activity of rhodopsin and several other related compounds (opsins). Rhodopsin is a modified form of vitamin A. During the process of light refraction and visual decoding, rhodopsin undergoes several transformations in response to photons, ultimately recycling itself in order to sustain continuous visual perception.
Signs & Symptoms of Vision Loss
All forms of vision loss produce different symptoms. Common signs and symptoms that warrant visiting the eye doctor include:
- Sleep-wake disturbances
- Visual anomalies such as blurred vision, color loss or spots in vision
- Reduced nighttime vision
- Migraines or headaches
- Dizziness, vertigo or loss of balance and coordination
- Nausea
- Disorientation
- Pressure, irritation or discomfort in or near the eyes
- Excessively dry or weepy eyes
Types of Vision Loss
Vision loss is generally associated with aging, a build-up of various materials in the eyes and a reduced capacity for cellular repair. Rarer forms of vision impairment and blindness are typically genetic.
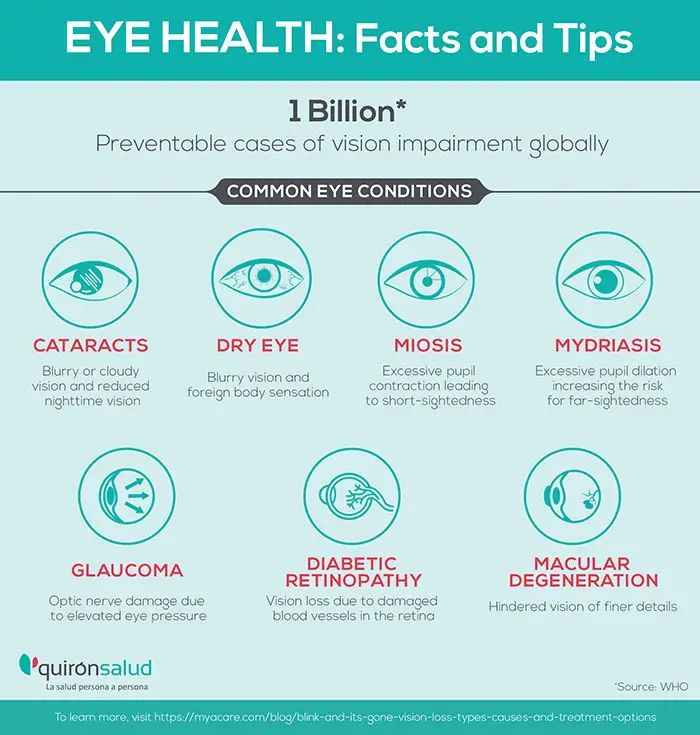
Common Eyesight Diseases
The following four diseases are the most common eye afflictions to affect the elderly population, often going hand-in-hand with other health conditions.
- Cataracts are dysfunctional deposits of protein in the lens of one or both of the eyes. It can cause one to be more sensitive to light, have reduced nighttime vision, as well as cause the vision to become blurry or cloudy. For many, cataracts are a normal part of the aging process. [4]
- Macular degeneration refers to the malfunction of the macula. The macula is the point at which light is focused onto the retina, being one of the most important components for seeing in fine detail[5]. There are two types of macula degeneration: wet and dry. The dry type is symptomatic of fat deposits in and around the macula that leads to its atrophy. The wet type describes excessive vascular growth and internal bleeding in the macula. Dry macular degeneration often progresses into wet macular degeneration.
- Diabetic retinopathy is a frequent complication seen in patients with diabetes. The blood vessels to the eyes, especially the retina, become malformed and damaged as a result of chronic insulin resistance and blood sugar spikes. In many with diabetes, symptoms of retinopathy are mild. However, they may progress rapidly towards blindness during the late stages of the disease.[6] Glaucoma and cataracts are other eye disorders that can arise from diabetic retinopathy.
- Glaucoma is an eye disease in which the optic nerve becomes progressively more damaged due to elevated pressure inside the eye. The eye typically overproduces or underdrains aqueous humor in this condition, contributing to increased pressure. Several types of glaucoma are known, the most common of which is open-angle glaucoma.
- Mydriasis. This disorder refers to the impairment of parasympathetic innervation to the eye and/or the overstimulation of sympathetic innervation. This causes excessive pupil dilation and increases the risk for far-sightedness.
- Miosis is the opposite disorder to mydriasis, resulting in excessive pupil contraction due to reduced sympathetic nervous system stimulation in the eyes. Having miosis is a risk factor for short-sightedness.
- Dry Eye is a condition that arises when your tears are unable to maintain adequate eye lubrication. This can be due to inadequate or poor quality tear production or the tears evaporating too quickly. Left untreated, impaired tear production can lead to eye infections and damage to the eyes' surface, including vision loss.
Refractive Error Disorders
Refractive error disorders refer to conditions in which the eye battles to refract light properly, resulting in either short or long distance visual impairment. These are the most common disorders to affect people of all ages.
- Myopia (short-sightedness) is the result of having a long eyeball shape or a thicker lens than usual.
- Hyperopia (far-sightedness) occurs due to having a short eyeball shape or a thinner lens.
- Presbyopia refers to age-related far-sightedness. As one ages, the lens becomes stiffer, resulting in a difficulty with lens accommodation and a reduced ability to focus on nearby objects.[7]
- Astigmatism is an eye disorder characterized by blurred vision in general. Those with astigmatism cannot focus their eyes enough to see anything clearly, whether close or at a distance. Any of the above conditions, as well as other eye disorders, increases the risk of astigmatism.
Color-Related Visual Impairment
Any disease that affects the perception of color typically impacts the number and/or function of cones in the eye. These are responsible for capturing the waveforms of color.
- Color blindness (achromatopsia) is a genetic, autosomal recessive disorder that describes a total or partial loss of color perception as a result of cone impairment. Partial color loss is more prevalent, with a deficit in detecting either red (protanopia) or green (deuteranopia) being most common. Visual loss of blue is very rare. Men are more commonly affected than women as the genes encoding color detection reside on the X chromosome.
Difficulty seeing colors may be a symptom of other eye diseases, such as glaucoma or optic nerve disorders. In these cases, blue and yellow may look very similar to the patient.
Nighttime Vision Loss Disorders
The ability to see at night is reliant on the number and/or function of rods in the eye, which are sensitive to light intensity and play a role in accommodation during dim light conditions. Conditions that affect the rods of the eye typically also reduce one’s ability to perceive color alongside contrast.
- Retinitis Pigmentosa. This is a genetic disorder characterized by progressive degradation of the retina. The first manifestations occur as night blindness, however an individual with the condition typically goes on to develop total blindness.
- Congenital Stationary Night Blindness (CSNB). Another genetic disorder, CSNB affects rods but not cones, resulting in complete blindness at night. Studies highlight that the disorder often presents with dysfunctional rhodopsin and in some cases, the rods in the eye never stop emitting light, directly blocking nighttime vision.
Other
Giant cell arteritis[8] and other vascular disorders may significantly affect eyesight and even lead to blindness.
Some patients with advanced autoimmune disorders, neurological infections or neurodegenerative diseases may also experience vision loss as a consequence of damage to the visual cortex in the brain. Neuromyelitis optica is an example of an autoimmune demyelination disorder that affects the occipital lobe and results in blindness.[9]
Damage to the brainstem as a result of an accident or major injury may also cause vision impairment.
Vision Loss Risk Factors
Women appear to suffer from visual problems more often than men, averaging a 55% bias. Those who have a family history of vision impairment are also at a greater risk of developing a similar condition.
Other risk factors for vision loss include:
- Autoimmune diseases. Various autoimmune diseases increase the risk of vision loss, such as systemic lupus erythematosus[10], multiple sclerosis, pemphigus vulgaris and other bullous autoimmune diseases[11].
- Stress typically activates the sympathetic nervous system and promotes hypertension, both of which can detract from eyesight and promote visual impairments. Furthermore, chronic stress is known to result in insulin resistance and can promote diabetes as well as diabetic retinopathy.[12]
- Infection. Many infectious diseases can promote vision impairment and eventually lead to vision loss. Examples include HIV/AIDS[13], COVID-19[14], toxoplasmosis gondi[15], leprosy, tuberculosis, malaria, and shingles.[16]
- Excessive UV radiation exposure. UV radiation is known to increase oxidative stress in the eyes, which promotes damage. If excessive, chronic eye damage can contribute towards macular degeneration or cataract formation. Children are more sensitive to UV radiation. As much as 80% of our lifetime UV exposure occurs before age 18, before the structures in the eyes complete their development.[17]
- Diabetes. As explained above, diabetes is one of the most common causes of vision loss and blindness. Erratic blood sugar levels and insulin resistance can impair cellular growth mechanisms, giving rise to faulty blood vessels that are thinner and weaker.
- Cardiovascular disease. Inadequate blood flow, too much or too little coagulation can result in a buildup of unwanted matter in the eyes, which increases the risk of vision disorders. As these symptoms are classic of cardiovascular diseases, they all typically promote vision loss. Hypertension and hypercholesterolemia also serve as risk factors for vision loss as well as cardiovascular disease.
- Eye-Toxic Medications. Certain medications increase the risk for eye disease. Antidepressants, antihistamines and loop diuretics can promote hyperopia and presbyopia.
- Vitamin A deficiency results in vision loss, particularly nighttime vision loss. If severe enough, an individual may develop nighttime blindness.
- Excessive electronic device use. Making use of a digital device such as a television, computer or cellphone for too long can promote eye strain, reduce lens accommodation and increase the risk of presbyopia. Engaging in such activity tends to reduce the number of times one blinks, resulting in drier eyes as well. Intense light exposure may alter circadian rhythm and the eye’s response to shifts in light intensity.[18]
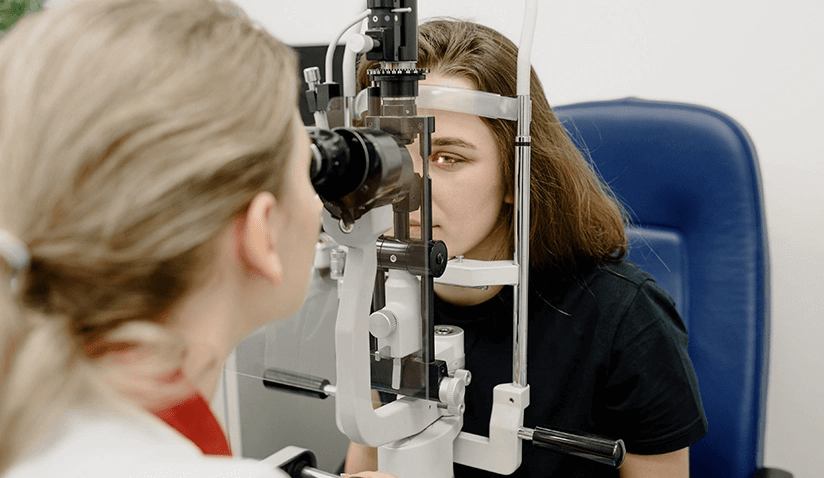
Eyesight Testing & Diagnostics
An ophthalmologist will first take a patient history and assess all potential risk factors for visual impairment. The patient will be asked about any visual symptoms, risk factors and family medical background.
Following this, the physician will have a better clue as to what tests will be required to assess the person’s vision. Before specific testing can take place, further basic screening will be carried out to rule out various possibilities.[19]
Preliminary Vision Testing
Preliminary vision testing includes a few quick, simple tests that an eye doctor will use in order to assess for vision anomalies. Often, a light will be shone in the patient's eyes in order to check that the pupils respond normally (contraction). The doctor may ask you to follow the movement of the light or an object to check that eye movement is regular. The alignment of the eyes can be checked simultaneously, all of which gives insight into the health of the eye muscles and lens.
Peripheral vision is also tested to rule out glaucoma and similar conditions in which this component of vision is lost. Using similar types of tests, your doctor may also check how well you can see different colors as well as depth perception and focus.
Visual Acuity Test
Visual acuity testing makes use of an eye chart in order to assess how well a person can see at a distance and up close. The results can ascertain whether a person is short-sighted, far-sighted or suffering from astigmatism (completely blurred vision). This is a standard test that is prescribed in many situations outside of the eye doctor’s office, such as when applying for a driving license.
If visual acuity is reduced, the ophthalmologist may then assess refractive status by redoing the test with a special device called a phoroptor. The phoroptor allows the doctor to test out multiple types of lenses in order to see what type of spectacles may improve the patient’s vision or not. The patient looks through the lens in the phoroptor and repeats the visual acuity test by reading the eye chart.
Inner Eye Examination
There are a number of devices and tests that an ophthalmologist may run in order to assess the function and health of the inner eye. Pupil-dilating eye drops are often employed in order to see past the superficial structures of the eye and to take a deeper look at both the retina and lens.
Slit-lamp microscope testing makes use of a special device that lights up and magnifies the eyes in order to highlight most parts of the eye. A temporary dye may be used to check for any damage on the surface of the eye.
Ophthalmoscopy refers to a retinal examination in which an ophthalmoscope is used to assess the health of the retina. The device shines an intensive light into the eye, and allows for the physician to see a detailed view of the retina and the back of the inner eye.
Tonometry
Tonometry is frequently used to check intraocular pressure or the pressure inside the eye. Often this test is used if glaucoma is suspected.
There are two main types[20]:
- Applanation tonometry makes use of pupil-dilating eyedrops as well as anesthetic in order to assess the force required to flatten the cornea (the outer surface layer of the eye). A slit-lamp microscope is used to press against the eye and to assess the pressure.
- Noncontact tonometry makes use of air to assess intraocular pressure. A blast of air is shot at the eye and the response is recorded. Unlike applanation tonometry, this type does not require anesthetic.
If eye pressure is normal, yet visual symptoms are indicative of eye pressure problems or glaucoma, then the doctor may check the thickness of the cornea using a pachymeter. Anesthetic is required for this test, which involves the momentary insertion of a probe into the cornea.
Eye Imaging
Aside from the above tests, the eye doctor may conduct more in-depth tests that provide detailed pictures of the inner eye in order to confirm a promising diagnosis.[21]
Examples include:
- Optical Coherence Tomography (OCT). OCT involves the use of a specialized laser device in order to take a cross section of the retina. This helps the optical specialist to ascertain whether the retina is too thick or thin and if it has any irregularities, such as growths or damage.[22]
- Fluorescein Angiography. This technique makes use of a special device that takes a high-definition image of the internal compartments of the eye. A dye (fluorescein) is injected into the arm beforehand and the pupils are artificially dilated. Once it reaches the eye, the dye makes the blood vessels and other structures in the eye fluorescent. The device takes a picture that the ophthalmologist can then use to add to their evaluation.[23]
Treatment Options
Vision loss is most commonly treated with an eyewear prescription. Eye disorders may be corrected through the use of medications and/or surgery.
Prescription Eyeglasses or Contact Lenses
Prescription eyewear is different to the spectacles one can buy over-the-counter in pharmacies, which are typically used for magnifying small text.
Instead, prescription glasses are scientifically designed to enhance vision in a number of ways through modifying the shape of the lens. Most prescriptions are for single vision lenses, which are either completely concave or convex in order to treat near-sightedness or far-sightedness respectively.
- Bifocal and trifocal lenses are a composite of these types of lenses. These types of lenses are often more expensive, however they are able to treat specific types of vision loss. They allow for the person to look through either one or the other, depending on if they need to see objects at close, intermediate or far distances (bifocals lack intermediate lenses). [24]
- Progressive lenses are often preferred as they are made to offer a smooth progression between these otherwise very distinct lens types.
Ocular Medications
There are a limited number of medications that are prescribed in order to treat eye disorders. Many of them treat other conditions that promote vision loss as opposed to treating the eye itself. Examples include:
- Injections. Vascular endothelial growth factor inhibitors have been prescribed for those with wet macular degeneration and other retina problems, such as diabetic retinopathy.[25]
- Medication. Prostaglandins, beta blockers, carbonic anhydrase inhibitors, and cholinergic drugs can all be prescribed for treating glaucoma.[26]
- Eye Drops. Prescription eye drops are prescribed to lower eye pressure in those with glaucoma and eye infections. In the case of an eye infection, antibiotic eye drops may be used for treatment. Eye drops also provide relief for those with dry eye syndrome.
- Supplemental Formulas. Various nutrients have been shown to slow the progression of macular degeneration, including vitamin C, E, zinc, copper and lutein.[27]
Surgery
There are many types of eye surgeries. The majority of them make use of laser technology. Examples include:
- LASIK. Laser In-Situ Keratomileusis or LASIK is one of the most common ocular surgeries. It can be used to treat many vision loss disorders, including astigmatism, far-sightedness and short-sightedness. LASIK works by making small laser incisions in the cornea and removing some of the inner contents, ultimately changing its shape.
- Photorefractive Keratectomy. This is considered a gentler laser surgery that LASIK. The cornea is reshaped through removing small amounts of tissue from the surface, as opposed to the inner layer.[28]
- Cataract Removal. Phacoemulsification surgery involves the use of an ultrasound or laser device that breaks up the cataract and lens. Following this, the lens fragments are removed and an artificial one is inserted. Extracapsular cataract surgery is another option for cataracts that are too dense to break apart. Instead, the entire lens is removed in one piece and replaced with an artificial one.
- Laser Trabeculoplasty. This surgery uses a laser device to reduce eye pressure in open-angle glaucoma before it advances towards irreversible vision loss.[29] The procedure slows the progression of the disease and may be repeated every couple of years when effects wear off.
Contraindications
Surgery is contraindicated for those with a history of diseases or infections that produce vision loss. Those who are subject to refractive instability, and that keep on needing new eyeglasses prescriptions, are also not good candidates.
As these surgeries run a small risk of making vision worse afterwards, it’s important to discuss with your ophthalmologist whether it’s worth the hassle.
Corneal Stem Cell Therapy and Beyond
Many visual diseases incur damage to various structures in the eyes, for which there is no known cure as of yet. Medications and supplements have been shown to slow down the progression of eye disease in some individuals, while corrective surgery and spectacles merely patch current symptoms.
Scientists are investigating ways in which the eyes can be repaired completely so that the prognosis for those with ocular damage can change.[30] One promising avenue is stem cell technology, in which these structures can be encouraged to regrow and completely regenerate. Preliminary trials have been showing great success, with one available stem cell therapy already available in top eye clinics around the globe.
- Holoclar is the only approved stem cell therapy for treating vision loss pertaining to cornea damage.[31] Damage to the cornea is known to cause outright blindness. Patients without stem cells are unable to have their sight restored through surgery alone. Stem cell implants have improved corneal surgery dramatically and have begun to restore cornea-related blindness and vision loss.
Studies indicate that it may be possible to restore other damaged parts of the eye, including the lens, retina, macula, rods and cones. More research is required to perfect this experimental approach in terms of stem cell delivery to the deeper parts of the eye and immune acceptance of foreign tissue.[32] In time, perfected stem cell technologies may be widely available, with blindness and vision loss being concerns of the past!
7 Eyesight Preservation Tips
Following the below tips can help to enhance and maintain optimal vision throughout one’s life.
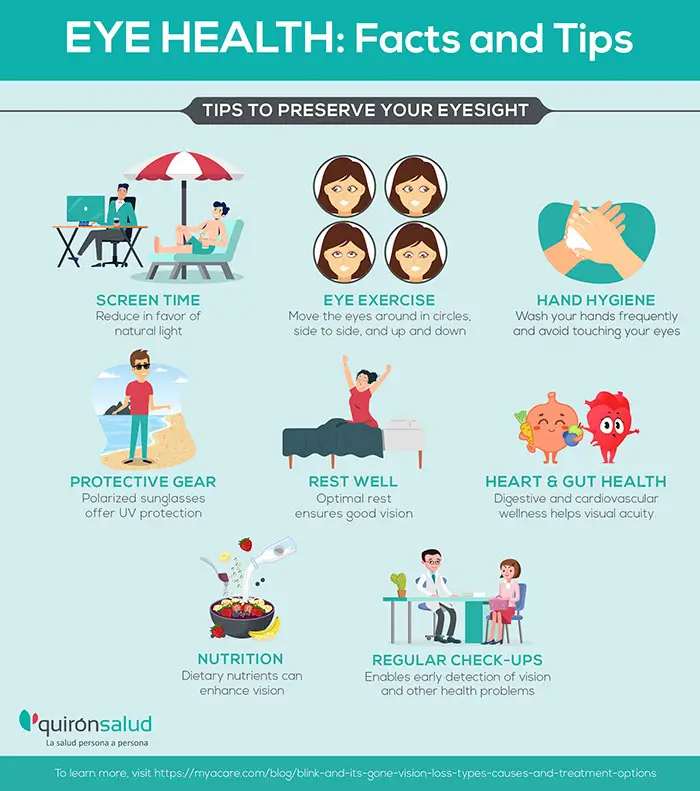
1. Digital Light Exposure
The quality of light one is exposed to is important for optimal eye function. Digital light sources tend to be a lot brighter than natural light sources, having an additive effect on vision over time. Furthermore, the type of light emitted is largely blue light[33], which is known to be more intensive on the eyes[34].
If one is required to spend a lot of time in front of electronic devices, or under conditions of artificial light, it’s then important to implement precaution in order to protect the eyes. Taking frequent breaks and opting for a natural source of light helps, as does maintaining a good body posture. For those who work at the computer, a larger font size may help to ease eye strain. Blue light blocking glasses are also available that may help to ease the effects of artificial light on the eyes and improve symptoms of digital eye strain.
Positioning oneself further away from the screen helps to alleviate accommodation deficits, where the eyes become lazy from overly focusing on a nearby object. Stopping to look outside a window at a faraway object can provide temporary relief for this type of eye strain and help to keep the muscles in the eye fit for vision accommodation.
2. Eye Exercise
Moving the eyes around in circles, from side to side, up and down, and so forth, serves to exercise the orbital muscles. Strengthening the orbital muscles in this manner improves lens accommodation and helps to optimize blood flow to the area, which may alleviate certain types of eye pressure.
A study carried out on 32 students revealed that eye exercises or “eye yoga” dramatically reduced symptoms of computer-related eye fatigue over the course of 6 weeks.[35]
Be careful not to move them too quickly or overdo it, as it may promote dizziness!
On this note, ordinary exercise increases blood flow to all areas of the body and can also help the health of the eyes. Regular exercise at a moderate intensity is best for preserving vision and overall well-being.
3. Hand Hygiene
Eye infections and ocular inflammation tend to occur as a result of rubbing or touching the eyes[36]. As this is a rather natural reflex, hand hygiene is vital to ensuring the eyes remain in good health.
This is particularly pertinent during the current covid pandemic as sars-cov-2 is known to infect the eyes and greatly increase the risk of vision anomalies[37]. On this note, make sure not to get disinfectant or other harsh chemical agents in your eyes, as they are one of the most sensitive organs in the entire body.
4. Protective Gear
Protective gear is very important for those exposed to occupational hazards. Lab workers, welders, and other laborers involved in industrial work that exposes the eyes to noxious fumes, irritants and chemicals ought to wear protective eye gear. Sailors and maritime workers may also wish to invest in eye protective gear due to being exposed to the harsh glare of the sun on the sea.
A Word on Sunglasses
Large polarized sunglasses can partially protect sensitive eyes from UV rays, with UV-resistant goggles providing the best protection[38]. Sunglasses coupled with a hat can optimize the protection sunglasses provide.
While offering this partial protection, prolonged use of sunglasses may not actually be the best for eyesight. Sunglasses may weaken the eye’s ability to adapt to changes in light intensity over time, as they promote a low-light environment. In bright light, the pupils contract, which serves to protect the lenses of each eye. Sunglasses are associated with decreased blinking and promoting pupil dilation, which may increase the amount of UV radiation exposure that the structures of the inner eye receive.[39]
5. Rest Well
Getting optimal rest at the right time is essential for maintaining good vision for one’s entire life. Sleep deprivation and poor sleep quality have been associated with reduced color vision[40] and visual acuity[41] [42].
Destressing is also an important point to make here, as being overly stressed and exhausted can lead to a loss of pupil contraction and lens accommodation. Tension may also detract from eye health by impacting blood flow to the eyes, as well as muscle contraction. Vision depends largely on the actions of sodium, which should be consumed in moderation to avoid visual anomalies and hypertension.
6. Focus on Metabolic and Cardiovascular Health
Metabolic diseases, such as diabetes and vascular abnormalities are some of the leading contributors to age-related vision impairment, including glaucoma, macular degeneration and blindness. In this respect, improving both digestive and cardiovascular health is likely to have a lasting impact on visual acuity.
Consuming balanced meals and healthy snacks at regular intervals helps to control blood sugar levels and blood pressure, as does moderating one’s salt and sugar intake. Managing stress levels is important, as chronic stress is known to interfere with insulin release and promote hypertension.
If you’re a smoker and you find your vision diminishing, quitting can go a long way towards improving your eyesight.
7. Nutritionally-Enriched Diet
While it remains to be conclusively proven, dietary nutrients do appear to have a beneficial impact on the health of the eye and may enhance aspects of vision.[43]
This is particularly true of antioxidants like vitamin C and E, which are associated with improved protection against lipid peroxidation. In macular degeneration, cataracts and diabetic retinopathy, fats are often misplaced and a cause of inflammation due to peroxidation.
The pigments of the eye that respond to light are made of various forms of vitamin A, including retinal, lutein and zeastaxanthin. In deficient individuals, these supplements may help to enhance symptoms of visual impairment.
While a diet enriched with these nutrients may help, there is no known cure for vision loss. A highly nutritious diet in general will also promote the health of the digestive and cardiovascular system, which in turn indirectly promotes eye health as well.
When to See an Eye Specialist
If a problem is suspected, it’s better to get an accurate diagnosis as soon as possible before it becomes unmanageable. According to a 30 year survey, eye care specialists and services helped to prevent age-related blindness in the global population.[44]
It’s important to seek the help of a qualified eye specialist when assessing visual health. A lot of institutions make use of untrained personnel to conduct visual acuity tests, which can create a false sense of security about one’s vision.[45]
Eye specialists fall into the following categories[46]:
- Ophthalmologist. An ophthalmologist is the most qualified type of eye doctor, having advanced medical training with additional specialization in eye health. They can offer in-depth diagnostics and treatment options for all forms of eye disease, including corrective surgery.
- Optometrist. Optometrists are like the general practitioners of eye health. They offer basic eye exams, prescribe glasses and contact lenses, as well as monitor the progression of vision disorders. An optometrist may refer the patient to an ophthalmologist when symptoms are severe or when surgery is indicated.
- Optician. An optician is not an eye doctor. Instead, they make custom lenses for eyeglasses and contact lenses. One needs to visit the optician after seeing an eye specialist and receiving a prescription for eyewear.
Conclusion
Vision is often taken for granted until symptoms of visual impairment start to set in! The eyes tend to suffer as a result of poor health and overexposure to visual risk factors. These include occupational hazards, excessive UV radiation, digital screen time and diseases which affect the cardiovascular system.
Safeguarding one’s health through consuming a nutritionally balanced diet, exercising and getting adequate sleep go a long way towards preserving one’s vision. Limiting screen time, using eye-protective gear and consulting with an eye doctor when visual symptoms make themselves clear have all been linked with longer-lasting visual acuity.

Dr. Carlos Vergés is the Head of Ophthalmology at Dexeus University Hospital (Quirónsalud). Specialized in Advanced Ophthalmology, Dr. Vergés and his team deliver cutting-edge technological, medical, and surgical expertise. After graduating in Medicine and Surgery from the Faculty of Medicine of the University of Barcelona, Dr. Vergés moved to Boston (USA) to pursue research in ophthalmology, completing a doctorate in Biology from Harvard University. His areas of interest focus on cataracts and the neurophysiological mechanisms of vision, especially those related to sports.

Dexeus University Hospital (Quirónsalud), also known as the 'Knowledge Hospital', is the center of reference in many of its specialties, being one of the first private university centers in all of Spain. The hospital has a solid team of more than 450 medical professionals and incorporates the latest functional and technological advances typical of leading centers. Every year, 49,000 hospital stays are registered, more than 85,000 emergencies are treated (about 230 daily), 10,000 plus surgical interventions are performed, and over 2,500 deliveries and around 50 clinical trials are carried out at the hospital. The Ophthalmological Institute at Dexeus University Hospital specializes in various fields of ophthalmology, utilizing the most modern technological equipment and advanced diagnostics. The team delivers comprehensive medical care and the most advanced surgical treatments for eye health. In addition, as vision problems are closely related to general health, they collaborate closely with medical specialties such as internal medicine, endocrinology and nutrition, rheumatology, gynecology, and others to offer comprehensive treatment.
Sources:
Featured Blogs



