Excretory System Overview

Medically Reviewed by Dr. Sony Sherpa (MBBS) - August 13, 2024
The excretory system is crucial for the survival of an organism, ensuring that all functions of the body are carried out effectively and efficiently. This system is primarily involved in the removal of waste products from the body. Without it, the body would become highly toxic and quickly succumb to a lethal disposition.
The following overview discusses the excretory system with a main emphasis on the urinary system, which is arguably the most important aspect of excretion.
Elimination vs. Excretion
Excretion is the disposal of waste products and forms a vital part of all biological cycles at the cellular level.
Cells take in nutrients and use them to produce functional products in response to cellular signals. Signals consist of a wide array of compounds, including hormones, microbial by-products and basic nutrients such as minerals, vitamins, amino acids and other peptides. Additionally nerve impulses and environmental cues such as temperature and pH affect certain cell cultures in ways that generate signals in response. Signaling compounds instruct the cell what products to produce from the building blocks it receives. They interact either directly or indirectly (via chain chemical reactions) with the cell’s DNA.
In this context, the excretory system can technically comprise every organ and system in the body. Thus the term elimination is used to describe cellular excretion – the waste products are typically eliminated from the cell and moved along to an organ that can process them.
Components of the Excretory System
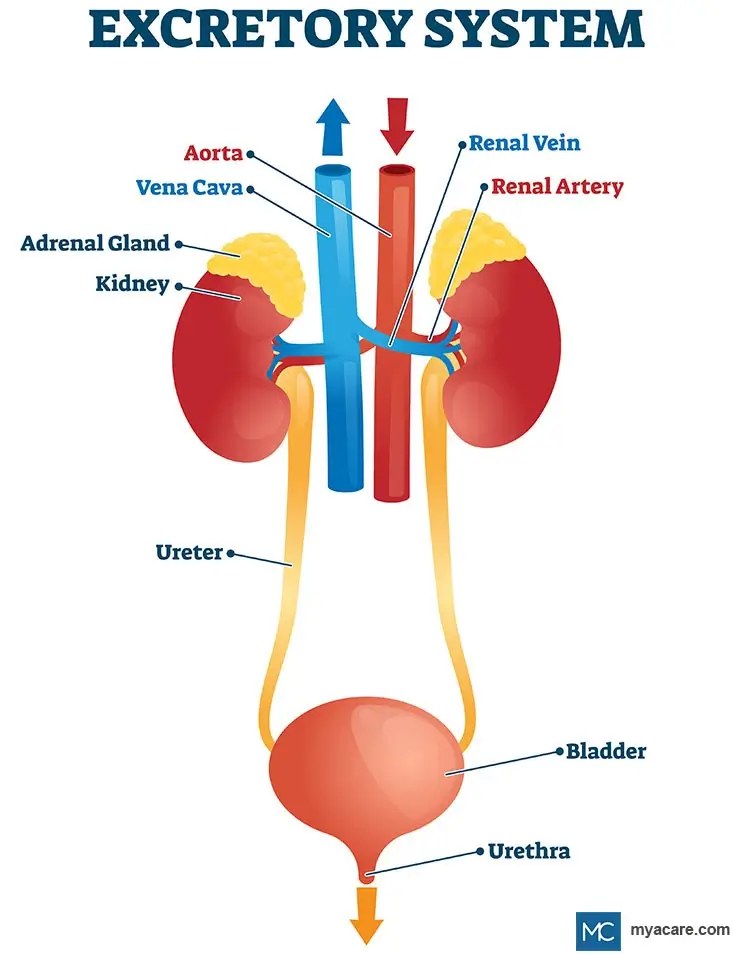
The main organs that process cellular waste products for excretion (complete removal from the body) are the kidneys, the digestive tract (mainly the colon and gut microbiome), the lungs and the skin. The bladder carries out the final excretion of urinary waste products that are refined in the kidneys, with both organs forming the urinary system.
The urinary system is perceived as being the most important part of the excretory system as a whole and is discussed below. The other systems involved in excretion are also reviewed.
The Urinary System
The urinary system is responsible for processing waste products from the blood, filtering them in the kidneys and excreting them via the ureter (tube connecting the kidneys to the bladder), bladder and urethra. Another name for the urinary system is the renal system.
Aside from the filtration and elimination of blood waste products, the renal system helps to maintain healthy blood pressure, blood pH, electrolyte balance and bodily osmosis (fluid homeostasis).
Kidneys
The kidneys take the majority of cellular waste from the body, transported to them via the bloodstream. They then produce urine and send it to the bladder for excretion.
Blood supply to the kidneys stems directly off of the main vein and artery that descend from the heart; reflective of the importance of these vital organs. The kidneys require optimal oxygenation for energy manufacture in order to maintain optimal homeostasis in the body.
Regulation of Kidney Function
The kidneys are regulated by hormones, nerve impulses as well as its own internal regulatory mechanisms.
1. Endocrine and Nervous System Regulation
The kidneys, like all bodily organs, are home to neuro-endocrine cells that send feedback to the brain, as well as those that receive it and alter kidney function.
The hypothalamus in the brain receives a wide variety of signals relevant to kidney function by monitoring nerve impulses and blood activity. In response to these stimuli, it sends signals to the pituitary which then in turn releases hormones that the kidney responds to by modulating its functions.
Nerve impulses are also generated that cause the smooth muscles in the kidneys to relax or contract, depending on the circulatory requirements of these excretory organs.
2. Auto-regulation
In the absence of neuro-endocrine involvement, the kidneys are still able to function and appear to have their own form of auto-regulation.
Auto-regulation is a homeostatic mechanism that is usually referred to in the context of the cardiovascular system, in which blood vessels relax or contract as a result of increased or decreased blood pressure respectively. When applied to the kidneys, auto-regulation of kidney blood vessels alters the rate at which it eliminates and recycles waste products, thereby regulating kidney function.
Kidney Function
The two main functions of the renal system are elimination and osmoregulation, which each simultaneously serve a variety of other functions when fulfilled by the kidneys[1].
1. Elimination
Elimination refers to the removal of waste products. In terms of kidney function, elimination refers to their removal from the bloodstream. The blood waste products it eliminates form urine which is then emptied into the bladder for final excretion. The kidneys filter approximately up to 200 L or 53 gallons of water from the blood every day![2]
A large portion of bodily waste is derived from the liver. The liver is involved in many processes pertaining to bio-transformation, in which nutrients or cellular metabolites are transformed into further useful products and waste products. Urea is synthesized primarily in the liver before it makes its way via the bloodstream to the kidneys and to a lesser extent, the skin.
Urea contains many hormonal by-products and proteins as well as lots of nitrogen, calcium and phosphorus. The kidneys filter through liver-derived urea before producing the final substance that is excreted during urination. Kidney-derived urea, or urine, also contains excess mineral ions from the blood stream at large, including all electrolytes (calcium, magnesium, sodium, potassium and chlorine) as well as any other blood minerals we may have in excess. Ammonia, uric acid, creatinine, pigments and inorganic salt also form part of urine.
The main active component of the kidney would be the nephrons, which are responsible for recycling useful waste products and eliminating unnecessary ones. Nephrons consist of intricate renal tubes which are designed to recycle metabolites in the blood and excrete the rest. Anything that can be recycled is typically sent back to the liver while the rest combines with water to produce urine. This is achieved through selective membrane permeability. Mineralocorticoids and certain other substances alter the permeability of the membranes inside nephrons.[3]
Different portions of each nephron are involved in different aspects of elimination. Nephrons are anatomically divided into the following sections[4]:
- The Glomerulus is a collection of very refined capillaries that feed blood into the kidneys. They form miniscule loops that feed into renal corpuscles. The glomerulus is actively involved in glomerular filtration, which serves to filter through waste products in the blood.
- Renal Corpuscles are tiny, yet bulbous structures that surround the capillary loops of the glomerulus. The part surrounding the glomerulus is called the glomerular capsule or Bowman’s capsule. Blood is allowed to fill the spaces around the glomerulus. A thin membrane separates this blood from urea and other waste products that move through to the internal compartment of the renal corpuscle, referred to as Bowman’s Space. Once blood is filtered, it passes back out of the kidneys and into circulation. Unfiltered blood enters renal corpuscles through the afferent arterioles and filtered blood leaves through efferent arterioles.
- Renal Tubules consist of the proximal convoluted tubule, the loop of henle and the distal convoluted tubule. These portions of the nephron further refine elimination and aid in osmoregulation. With the exception of the loop of henle, the cells lining these tubes have brush border villi, which participate in extracting any beneficial nutrients from the contents passing through the tubules. The efferent arteriole runs parallel to the renal tubules, participating in the exchange of metabolites, minerals and water to ensure adequate elimination.
- The Proximal Convoluted Tubule forms the first portion of the renal tubule and is characterized by several loops followed by a portion that descends before meeting the loop of henle. This portion is involved in the reabsorption of glucose, amino acids, ascorbic acid, lactic acid, uric acid, minerals, water and a few other compounds. It also actively works to secrete certain substances like penicillin, creatinine, histamine and charged hydrogen ions – the latter of which helps to maintain blood pH.
- The Loop of Henle continues to descend from the end of the proximal convoluted tubule, curving back upward to join the distal convoluted tubule. Most of this portion of the renal tubule is very thin and is only active in water reabsorption. A section of the ascending limb bulks up to match the size of the rest of the tubule and likewise, this section is involved in reabsorbing water, sodium, potassium and chlorine.
- The Distal Convoluted Tubule is responsible for secreting further waste products into the tubule contents, including acids, proteins and mineral ions. Sodium is reabsorbed from this portion of the tubule, as is water but only in the presence of antidiuretic hormone. Once the last of the waste products have been incorporated into the contents of the renal tubule and the useful ones reabsorbed, the fluid left over is urine.
- Collecting Ducts technically do not form part of nephrons, but are nonetheless continuous with them. They eliminate urine from the nephron by emptying it into the ureter for transportation to the bladder.
While similar in function, there are two types of nephron. Each contain the same parts, however they are located in different regions of the kidney. Most of the nephrons in the kidney are cortical nephrons, involved in the production of urine. Closer to where blood leaves the kidneys reside the juxta medullary nephrons which receive urine from cortical nephrons and concentrate it. These nephrons only comprise up to 15% of the nephrons inside the kidney, with cortical nephrons making up the rest.
2. Hormone Production
The kidneys are responsible for generating a small pool of hormones that govern osmosis, blood pressure, electrolyte balance and more. These hormones include:
- Renin which is required for osmoregulation, forming part of the renin-angiotensin system.
- Erthropoietin Hormone which stimulates the growth and development of red blood cells from stem cells in the bone marrow.
- 25-Dihydroxycholecalciferol (Vitamin D3) which is an active form of vitamin D. Vitamin D3 is known as a pro-hormone, meaning that it has hormonal actions and the scope of these actions is vast throughout the entire body. Calcium homeostasis, the immune system, growth and development as well as cellular energy production are regulated in part by the actions of vitamin D3. This vitamin can only be produced in the body from the degradation of cholecalciferol in the skin, an event that occurs during exposure to sunlight.
3. Osmoregulation
The kidneys regulate the balance of fluids in the body through being in control of mineral re-absorption and excretion. [5]
Mineral ions govern the movement of fluids in and out of cells, being the master coordinators of osmosis in the body. Thus, disturbances in the balance of cellular (internal) and blood (external) mineral concentrations determines how much water the kidneys withhold to maintain osmoregularity. Sodium and potassium are the main regulators of water retention. Water levels are also involved in conserving blood volume, a factor that is intimately linked with cardiovascular function and blood pressure.
Osmoregulation is further governed by a group of hormones produced at various sites of the body. These hormones include:
- Renin is produced in the kidneys and is required by the renin-angiotensin system to regulate osmosis, blood pressure and blood volume. Renin chemically breaks down angiotensinogen, a substance that the liver and kidneys produce in order to create angiotensin. Other organs can also produce angiotensinogen, suggesting that the rest of the body may also be involved in regulating kidney function and blood pressure. It is also possible that this precursor is involved in blood vessel growth, yet evidence is inconclusive[6]. Renin is triggered in response to lowered renal blood pressure or low sodium levels in the renal tubules.[7]
- Angiotensin I and II are created from the interactions of renin and angiotensinogen, a protein made in the liver. Renin transforms angiotensinogen into angiotensin I, which is then further converted into angiotensin II by Angiotensin- Converting Enzyme[8]. Angiotensin II constricts blood vessels in order to maintain optimal blood pressure. When levels of angiotensin II are high, renin production is low and vice versa. Angiotensin II stimulates more blood flow into the kidneys through promoting vasodilation and more sodium absorption via promoting aldosterone production. In contrast, the blood vessels outside of the kidney respond to angiontensin II by constricting, resulting in an increase in blood pressure. This hormone also binds acts in the hypothalamus to increase the sensation of thirst, as well as water consumption.
- Aldosterone is an adrenal hormone that is released in response to angiotensin II. It works to increase sodium reabsorption by modulating the mineral balance inside the kidneys. Aldosterone is known as a mineralocorticoid in this respect.
- Antidiuretic Hormone is released from the pituitary in response to hypothalamic osmotic feedback, subsequent signaling and blood levels of angiotensin II. This hormone acts on the nephrons of the kidneys, instructing them to increase permeability in the collecting ducts and to reabsorb more water. This increases bodily water retention and concentrates or even withholds urine.
Other hormones can also affect kidney function, such as endothelin (a vascular protein) and norepinephrine which promote vasoconstriction and a decrease in the filtration rate. Nitric oxide, inflammatory cytokines, neurotransmitters (like dopamine) and histamine serve as vasoconstrictors, increasing the filtration rate.
Bladder
The bladder is an organ that takes urine from the kidneys via the ureter, storing it until urination is possible. The thick membrane of the bladder comprises of three layers of muscle tissue known as the detrusor muscle, which facilitates its functions. It also contains two sphincters that sit underneath the organ, connecting the urethra to the bladder.
Bladder Function
The bladder serves two main functions, with a potential third function[9]:
1. Storage
When the bladder is not in use, the detrusor muscle remains relaxed while the sphincters remain contracted. This ensures that urine remains inside the bladder, storing it until excretion takes place. Storage of urine is particularly important during the night when we’re asleep in order to promote better rest and rejuvenation.
Bladder volume and pressure are controlled through the nervous system via the actions of neuro-endocrine cells, neurons and nerve impulses. When pressure in the bladder rises due to urinary retention, nerves connected to the bladder relay sensory information to the brain via the pelvic girdle and spinal cord. Through this feedback, we become aware that we need to urinate. Other nerve fibers respond to other signals, such as chemical irritation, similarly alerting the brain which then acts to mediate bladder function appropriately.
2. Excretion
During urination, the sphincters relax and open, while the bladder contracts alongside relevant portions of the urethra, facilitating urinary excretion. The contraction of the bladder also pinches closed the opening to the ureters, ensuring that the kidneys don’t experience urinary reflux during urinary excretion.
Aside from being governed via central nervous system feedback, urination is also governed by the peripheral nervous system. The sympathetic nervous system prevents urination from occurring and the parasympathetic nervous system encourages it. In this respect, feeling stressed can cause urinary retention while being relaxed promotes better urinary function.
3. Water and Metabolite Reabsorption
Originally, the bladder was thought of merely as a storage and excretion organ. However in recent years, evidence has surfaced that reveals that the cells of the bladder are able to absorb water from stored urine[10], thus increasing its concentration of waste products and conserving bodily water. In animal studies, it is shown that the bladder also reabsorbs nitrogen and creatinine[11].
Other Organ Systems Involved in Excretion
The following systems also play a role in the excretory system, however the role is minor compared with the processing capacity of the urinary system.
Digestive System
The digestive system is involved in the excretion of waste products in the form of defecation. Digestive waste, better known as feces, comprises of excess hormones, minerals, dietary metabolites, undigested food, microbial waste and other by-products the body does not need.
Through the process of digestion, water and nutrients are absorbed from digesting food that moves through the digestive tract. The tract is broken down into the stomach, the colon, the small intestine, the large intestine and the rectum. Contractions along the muscles of the digestive tract are responsible for the movement of food and waste, known as peristalsis.
When waste products reach the end of the tract and enter the rectum, expansion of the rectal walls informs the nervous system and alerts the organism that it needs to defecate. If the urge is denied for longer than a minute or two, the feces move back into the digestive tract where more water is extracted from them. Prolonged fecal retention causes constipation and eventually contributes to systemic toxicity.[12]
Respiratory System
The lungs mostly serve to help us to breathe. The act of exhaling is also an act of gaseous excretion.
The lungs have a very large surface area in order to oxygenate enough blood to sustain the energy requirements of the body. The surface area also helps to expel all gaseous waste products from the blood, with the exception of microbial ones from the gut which are released via flatulence.
The main waste products that the lungs excrete consist of carbon dioxide and water. This requires charged hydrogen ions and bicarbonate ions to execute.[13]
Skin and the Integumentary System
The skin’s main function is to protect the internal environment from external threats[14]. Its secondary functions lend toward temperature regulation and excretion via sweating.
The main aim of sweat is to cool the body down[15], however, and it only plays a minor role in the excretory system. Mineral salts, especially sodium, and water are the main components of sweat, with a small portion consisting of proteins, hormone metabolites (think pheromones), vitamins, viral by-products and a few other toxic substances[16]. Sweat glands also excrete a fraction of liver-derived urea in the form of sweat.
To search for the best healthcare providers worldwide, please use the Mya Care search engine.
The Mya Care Editorial Team comprises medical doctors and qualified professionals with a background in healthcare, dedicated to delivering trustworthy, evidence-based health content.
Our team draws on authoritative sources, including systematic reviews published in top-tier medical journals, the latest academic and professional books by renowned experts, and official guidelines from authoritative global health organizations. This rigorous process ensures every article reflects current medical standards and is regularly updated to include the latest healthcare insights.

Dr. Sony Sherpa completed her MBBS at Guangzhou Medical University, China. She is a resident doctor, researcher, and medical writer who believes in the importance of accessible, quality healthcare for everyone. Her work in the healthcare field is focused on improving the well-being of individuals and communities, ensuring they receive the necessary care and support for a healthy and fulfilling life.
Sources:
Featured Blogs



