Heart Failure: The Latest in Diagnostic Tools

Heart failure, also termed cardiomyopathy, is a progressive condition where your heart fails to pump blood adequately for your bodily needs. Globally, it is one of the top causes of hospitalization, per the World Heart Foundation. According to the WHO, cardiovascular diseases remain the number one cause of mortality in Germany and worldwide.
In recent times, the global incidence of heart failure has risen to approximately 26 million. Worrying as it is, many cases remain undiagnosed.
Coronary disease, hypertension, and valve-related problems are regarded as some of the top causes of cardiomyopathy. Heart failure is often associated with difficulty in breathing, leg swelling, and other symptoms inclined to worsen with exercise.
What is Heart Failure?
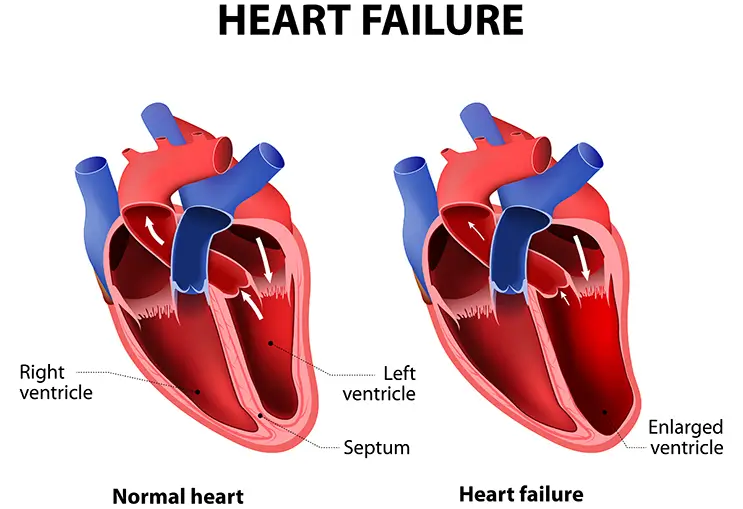
Heart failure is a cardiac condition that develops over many years and progresses with time. Having heart failure signifies a deficit in the blood volume pumped by the heart compared to the oxygen requirements of the body (e.g. organs, muscles, tissue, etc.).
Heart Failure is influenced by many factors, such as high blood pressure and coronary heart disease. These conditions, among others, will lead to weakness or stiffening of the heart muscle. Consequently, the heart fails to fill its chambers properly with blood and pump adequately throughout the body.
There are several types and classifications of heart failure, typically identified by heart imaging (e.g. echocardiography).
The emergence of heart failure can be gradual (chronic) or sudden (acute).
What Causes Heart Failure?
Several conditions that damage the heart can result in heart failure.
Typically, in cases of chronic heart failure, multiple conditions - rather than a single cause - affect the heart's ability to pump blood effectively around the body. Hypertension and coronary artery disease are two common causes of chronic heart failure.
Other possible causes include:
- Cardiomyopathy
- Abnormal heart rhythm
- Heart valve disease
- Congenital heart disease
- Diabetes
- Thyroid disease
- Viral infections impacting the heart. E.g. Myocarditis
- Certain medications and chemicals. E.g. Chemotherapy drugs
- Anemia
- Excessive intake of alcohol
On the other hand, acute heart failure leads to a sudden, rapid deterioration in cardiac functioning, affecting the amount of blood your heart can pump to the rest of your body.
The following factors contribute to the risk for sudden-onset heart failure - some in common with the chronic kind:
- Pulmonary embolism
- Diabetes
- Hypertension
- Hyperthyroidism
- End-stage renal disease
- Sleep apnea
- Stroke
- Viral infections that affect the heart. E.g. COVID-19
- Immoderate alcohol consumption
Certain existing heart conditions can also result in sudden-onset heart failure, such as:
- Arrhythmia
- Coronary artery disease
- Heart valve disease
Acute heart failure can often be reversible if the primary cause is managed properly.
Symptoms of Heart Failure
The main ones include:
- Shortness of breath (dyspnea): When the heart fails to deliver adequate oxygen to your body, your lungs will try to compensate for the deficiency. Dyspnea is usually worse with exercise and can be present even at rest in advanced or acutely decompensated heart failure.
- Edema (Swelling): Blood stagnates in the circulation since the heart is not pumping well, leading to congestion and edema. Swelling is most apparent in the legs since they are farthest away from the heart.
- Dyspnea when lying flat on the back: People with heart failure often sleep with several pillows under their head to breathe comfortably.
- General lack of energy and chronic fatigue
- Long-standing cough
These symptoms tend to slowly worsen with time in people who have chronic heart failure. Moreover, certain conditions, like a new heart attack or an infection, can lead to acute decompensation. This means that the already failing heart function quickly deteriorates, leading to acute worsening of your symptoms.
How Is Heart Failure Diagnosed?
There are many tools to diagnose heart failure to determine the type, grade, and severity. One or more tests may be required depending on the cause and type of cardiomyopathy. As with any health condition, early diagnosis improves outcomes, so it is important to seek the help of a doctor if you are experiencing any of the symptoms above.
Cardiac Imaging
Cardiac imaging is the mainstay of diagnosis in heart failure. It allows cardiologists to:
- Assess the function of the heart based on Ejection Fraction (EF). Sciencedirect.com defines EF as the percentage of blood volume ejected in each cardiac cycle. Ejection fraction can be a measure of right or left heart function i.e. right ventricular ejection fraction (RVEF) and left ventricular ejection fraction (LVEF). LVEF refers to the performance of the left ventricle in the systolic phase (when the ventricles contract) of the cardiac cycle, pumping blood into the circulatory system. RVEF measures the amount of blood pumped out of the right side of the heart to the lungs (into pulmonary circulation).
- Assess muscle movement
- Assess the coronary arteries
- Assess the diastole
- Assess the valve
Cardiac imaging supports clinical decision-making, helping to provide the most accurate and effective therapy available.
Highly specialized heart centers utilize high-end cardiac imaging and state-of-the-art technologies, such as:
3D Transthoracic Echocardiography
Transthoracic echocardiography (TTE) is a non-invasive heart imaging technique that uses sound waves to observe the heart as it pumps in real-time.
Advanced devices allow 3D reconstruction of the heart with speckle tracking (STE), giving more insight into the heart function and anatomy.
3D TTE utilizes a handheld sonar device moved on your chest. It’s a non-painful procedure that requires no anesthesia.
Transesophageal Echocardiography
Also called TEE. It’s similar to TTE, however, it is a semi-invasive diagnostic tool. In Transesophageal Echocardiography, a thin ultrasound probe needs to be advanced through the mouth to the level of the heart.
TEE sometimes requires sedation. Nevertheless, it allows for a more thorough assessment.
Stress Echocardiography
Stress Echocardiography is an established technique for dynamic assessment of cardiac structure and function. It uses physical (exercise), pharmacological, or electrical stress in combination with 2D echocardiography to identify new cardiac wall motion abnormalities, heart muscle damage due to heart attack or heart disease, as well as valve disease (E.g. dynamic mitral regurgitation) in some scenarios.
Cardiac CT
Cardiac Computed Tomography (CT) is an advanced non-invasive diagnostic tool for heart failure and coronary heart disease. It gives an extremely detailed view of the heart and coronary vessels. Cardiac CT also allows your team to calculate different scores and determine your risk of future cardiac events.
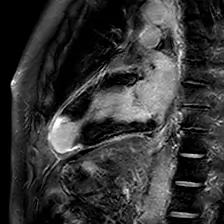
Cardiac MRI
Magnetic Resonance Imaging (MRI) is relatively new in the field of cardiology. It is utilized to complement other tests delivering a lot of insight into challenging cases that cannot be fully assessed with other techniques.
Single-photon Emission Computed Tomography (SPECT) and Radionuclide Ventriculography
The American Heart Association defines a SPECT scan as a noninvasive nuclear imaging test using radioactive tracers injected into the blood to produce images of the heart aided by a special gamma camera. A SPECT scan provides insights on blood flow to the heart, how well the heart is pumping, blood flow in your heart at rest or while exercising, and arterial narrowing. The radionuclide ventriculography (RNV) scan assesses blood flow patterns and the functioning of the right and left ventricles, thereby guiding precise intervention in cases of heart failure. As the name suggests, it is a nuclear medicine test using radioactive tracers.
Positron Emission Tomography (PET)
A PET scan utilizes radionuclides (nuclear tracers) to produce pictures of the heart at work. The scan shows if the heart is receiving adequate blood or if blood flow is reduced due to arterial narrowing. Dead cells or scars from a prior heart attack can also be identified. The injured but viable cardiac muscles revealed by the scan could be saved by interventional surgery to restore blood flow. A PET scan thus also helps determine if a cardiac procedure or surgery might be beneficial.
Heart Catheterization
Heart catheterization involves inserting a catheter through an arm or leg vein and advancing it to the heart. A dye is then injected, and an X-ray machine takes real-time images of the heart. This allows our cardiologists to measure different heart functions and the patency of the coronaries.
Cardiac catheterization can effectively assess and manage the most complicated cases of heart failure and coronary heart disease. Top centers have cath labs utilizing the most advanced technologies science and engineering have to offer.
Examples include rotational angiography, dynamic CT, Digital Subtraction Angiography (DSA), Fractional Flow Reserve (FFR) Measurement, Intravascular Ultrasound (IVUS), Electrophysiology and 3D Mapping. These technologies are available in our institution.
Laboratory Technology
B-type natriuretic peptide (BNP) is a hormone and N-terminal prohormone BNP (NT-proBNP) a non-active prohormone released by the heart in response to changes in internal pressure. An increase in levels can relate to heart failure in most cases. A blood test measures BNP and NT-proBNP levels that aid in diagnosing and monitoring heart failure.
Other Diagnostic Tests
These tests give your cardiologist a general idea about your heart function and health.
- Routine blood tests: Cardiac failure cannot be diagnosed by a specific blood test, however, some tests help to evaluate the problem and guide clinical decision-making.
- Electrocardiogram (ECG): Using electrodes attached to the chest, the electric flow in the heart can be assessed. It can show signs of coronary heart disease and heart failure.
- Chest X-ray: This can show signs of congestion in the lungs
If you suspect that you might have heart failure, do not delay consulting with a cardiologist. Proper diagnosis and treatment can significantly improve your quality of life and slow down the progression of the illness.

Professor Dr. Fabian Knebel is the Head of the Department for Internal Medicine with a focus on cardiology at Sana Hospital Lichtenberg and is dedicated to the diagnosis and treatment of cardiovascular diseases. He has also acquired extensive additional qualifications in the fields of interventional cardiology and cardiac insufficiency at the German Society for Cardiology (DGK).
Sana’s Cardiology Department in Lichtenberg is one of the top certified heart failure centers with a leading position in Germany and Europe.
Our team, led by Prof. Dr. Knebel, offers the most advanced diagnostic and therapeutic techniques. Our accredited heart imaging division offers patients access to the latest cardiac imaging techniques. 3-Dimensional echocardiography, cardiac MRI, and coronary CT scans allow our team to thoroughly assess heart function in a way that was not possible before. Cardiac imaging at Sana Hospital Lichtenberg (Berlin) is performed in collaboration with Prof. Dr. Sven Mutze and Dr. Christopher Nauck from the radiology department. By using various diagnostic imaging methods and applying a complex RIS/PACS system, diagnostic imaging is designed to be as effective and comfortable as possible.
Sources:
Featured Blogs



