The Vagus Nerve: What Is It, and What Issues Affect It?
How the Vagus Nerve Can Be Damaged
Symptoms of Vagus Nerve Dysfunction
The vagus nerve is an important nerve comprising about 75% of the nervous tissue of the parasympathetic nervous system. This is the division of the nervous system that is responsible for regulating many bodily functions. It works in conjunction with the sympathetic nervous system to regulate organ function and maintain homeostasis.
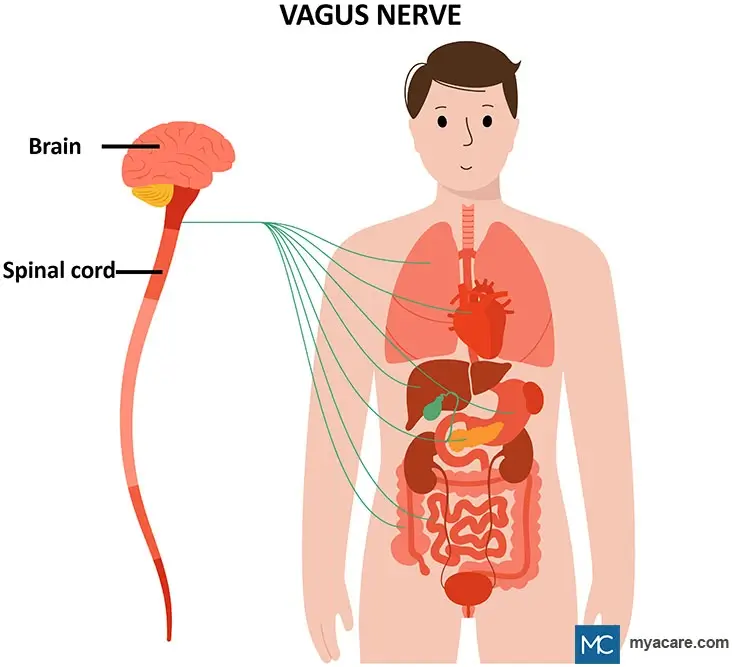
The vagus nerve transmits impulses between many organs such as the heart, lungs, stomach, pancreas, liver, and intestines to the brain and spinal cord and back again (refer to the image below).
Anatomy of the Vagus Nerve
The vagus nerve originates from the brainstem and is known as the tenth cranial nerve. The vagus nerve leaves the medulla oblongata of the brain and passes through an opening, the jugular foramen, situated between the skull bones.
The vagus nerve is mixed in the sense that it has both sensory and motor neurons. There are also two ganglia. A ganglion is a collection of nerves. Below we have a list of the branches of the vagus nerve and the organs they impact.
- The superior ganglia send nerves to parts of the ear.
- The inferior ganglia send nerve branches to the pharynx and larynx.
- The nerve continues past the ganglia and into the chest area, branching into the muscles of the esophagus and the heart and entering the lungs via nerve plexuses.
- Other branches of the vagus nerve enter the connective tissue layers of the gut, the stomach and both the small and large intestines.
How the Vagus Nerve Works
Information about the organs is sent by way of afferent nerve fibers. These are fibers that take information from sensory receptors and send the nerve impulse back to the brain. The vagus nerve has both motor and sensory functions. In other words, signals pass to the brain from organs but also return from the brain back to the organs.
Generally, sensory nerves convey sensory information while motor nerves bring about some type of response, such as muscle contraction and glandular secretion. The vagus nerve brings about involuntary actions; in other words, it causes actions that you have no conscious control over. It works antagonistically against the sympathetic nervous system. For example, while the sympathetic nerves speed up the heart rate, the vagus nerve slows down the heart rate.
Functions of the Vagus Nerve
The vagus nerve is essential for the normal functioning of many organs and structures of the body. It does also control many reflex functions including the gag reflex. The functions of the vagus nerve in each of the structures it innervates are given below.
- Brain: The vagus nerve impacts mood and appears to influence the connection between biota in the gut and the brain.
- Taste: The vagus nerve is one of the nerves involved in the taste sensation found at the back of the tongue.
- Pharynx and larynx: The nerve helps in voice production and swallowing activity.
- Heart: It decreases the heart rate and blood pressure.
- Lungs: It helps control breathing.
- Stomach: It sends a message to the stomach to contract to push food into the intestines.
- Pancreas: The vagus nerve influences enzyme secretions.
- Liver: It helps regulate glucose production by the liver in times of need.
- Intestines: It controls the secretion of substances from glands and helps the smooth muscles to contract when needed to push digested food along.
How the Vagus Nerve Can be Damaged
The vagus nerve can become damaged in a variety of ways. These are listed and described below.
- Viruses: Herpes simplex type I virus can cause a transient paralysis of the vagus nerve; in one patient this caused problems in swallowing and speaking. Even the COVID-19 virus has shown a negative impact on the vagal nerve.
- Diabetes: Poorly controlled blood sugar can result in vagus nerve damage.
- Scleroderma: This is an autoimmune disorder that impacts connective tissues throughout the body, even affecting the sympathetic and vagal systems involved in the functioning of the esophagus.
- Surgical complications: A mishap during surgery could compromise the functioning of the vagus nerve.
Symptoms of Vagus Nerve Dysfunction
There are several signs that the vagus nerve may not be functioning correctly. These are listed below.
- No gag reflex: This is also called the pharyngeal reflex and occurs when something touches the back of the throat.
- Dysphagia: This is when a person finds it difficult to swallow.
- Vocal problems: A person may be unable to speak or their voice may sound hoarse.
- GERD: Gastroesophageal reflux disease is the condition causing heartburn and reflux of acid from the stomach into the esophagus.
- Abdominal bloat: The person feels full quickly and experiences bloating and pain in their abdomen.
- Nausea and Vomiting: The person feels and becomes ill.
- Lack of appetite: The person does not feel hungry.
- Syncope: Fainting is common in cases of vagus nerve dysfunction.
- Dizziness: A person may feel dizzy with vagus nerve dysfunction.
Damage to the vagus nerve can result in gastroparesis, in which food does not easily move from the stomach into the intestine. This can cause the gastrointestinal symptoms mentioned above.
Vasovagal syncope is a condition found in some people who faint when their blood pressure drops or due to emotional stress.
Treatment for Vagus Nerve Issues
Vagus nerve stimulation (VNS) can be helpful in treating depression, anxiety, and seizure disorders like epilepsy. Stimulating the vagus nerve even helps reduce the symptoms of tinnitus and reduces nociceptor responses (painful sensations). This is why VNS is approved to treat migraines and cluster headaches. Medication can help improve motility and nausea associated with gastroparesis.
Conclusion
The vagus nerve is a cranial nerve that has many important functions in the body including regulating the heart rate, and digestion, and is involved in the gut-brain interaction. Problems with the vagus nerve can result in debilitating symptoms but treatment by VNS or medication can be helpful for patients.
To search for the best doctors and healthcare providers worldwide, please use the Mya Care search engine.

Dr. Rae Osborn has a Ph.D. in Biology from the University of Texas at Arlington. She was a tenured Associate Professor of Biology at Northwestern State University, where she taught many courses to Pre-nursing and Pre-medical students. She has written extensively on medical conditions and healthy lifestyle topics, including nutrition. She is from South Africa but lived and taught in the United States for 18 years.
Sources:
Featured Blogs



