How Do Trigger Point Injections Work?
Medically Reviewed by Dr. Sony Sherpa (MBBS) - July 01, 2022
An array of factors can cause muscle pain or myalgia. From sleeping in the wrong position to injury, infections, diseases, or the aftermath of an intense workout session, many things can trigger these aches.
Muscle pain can be short-term and frequently resolve after a few days of rest and recovery. However, some kinds of pain are chronic and have a significant impact on the quality of life and the ability to function. These kinds of pain may require medical treatment.
Many therapies help with chronic painful conditions. One such minimally invasive technique is trigger point injections.
Here we will talk about what are trigger point injections and why doctors use them. We will also see if you are a good candidate for it and what you should expect after the treatment. Then we will go on to answer some of your most frequently asked questions.
Let’s start from the basics!
What are Trigger Point Injections?
A trigger point injection (TPI) is a pain management procedure that is used to treat painful areas that contain trigger points.
These are highly sensitive knots of fibers in tight bands of muscles. The knotted fibers restrict blood flow to the muscles, and it keeps them tight and stiff, causing pain and a restricted range of motion. It also impacts the muscle’s willingness to stretch or contract, making movements painful.
Trigger points may be due to:
- Muscle tension.
- Pinched spinal nerves.
- Traumatic injury.
- Muscle over-exertion.
- Muscle spasms.
- Inflamed or injured tendons or ligaments or muscle fascia.
- Muscle inflammation.
- Past surgery.
- Muscle overuse, as a result of repetitive movements.
- Poor posture.
The rhomboid and trapezius back muscles, located in the upper back and behind the shoulder areas, are common sites of trigger points. Sometimes you can feel these knots when you rub these muscles.
In addition to the upper spine, trigger points can also occur in the low back or less commonly in the extremities. The area is tender, and the pain radiates from the trigger point itself to an area around it when pushed.
A TPI can help soothe muscle pain, especially in areas like your neck, lower back, arms, and legs. They can even be utilized to ease pain resulting from fibromyalgia, myofascial pain, and tension headaches.
The technique involves the injection of medications directly into myofascial trigger points. Your doctor will determine the best type of medicine based on the severity and underlying cause of the pain. Usually, these are pain-relieving medications but are sometimes combined with a drug that controls the underlying inflammation.
Who Can Get Trigger Point Injections?
Trigger point injections can help relieve chronic pain caused by musculoskeletal and nervous system disorders such as:
- Fibromyalgia.
- Myofascial pain syndrome.
- Headaches.
- Sciatica.
- Temperomandibular pain.
- Any other chronic condition that results in widespread pain.
- Sleep abnormalities.
- Distress.
- Fatigue.
- Chronic pelvic pain syndrome (it involves chronic prostatitis, painful bladder syndrome, interstitial cystitis, other urinary tract symptoms, and sexual dysfunction)
Let’s look at some of these in detail.
Fibromyalgia
This is a long-term condition that causes pain all over the body. It also causes increased sensitivity to pain, fatigue, sleep problems, and mental along with emotional distress.
The exact cause of fibromyalgia is unknown, but it is believed that abnormal levels of certain chemicals in the brain, nerves, and spinal cord cause alterations in the way pain messages are carried around the body.
Myofascial Pain Syndrome
Myofascial pain syndrome (MFPS), is a chronic pain disorder involving tissues that surrounds muscle (Myo means muscle and fascial means fascia).
In MFPS, trigger points stimulate pain responses in unrelated parts of the body which is called referred pain. This could be due to repetitive motion, poor posture, psychological stress, or injury.
Headaches
Migraine and tension-type headaches can be triggered by points in the head, neck, and shoulders.
Research has found a significantly higher number of myofascial trigger points in people with migraine as compared to those without.
What Medicine is Used in a Trigger Point Injection?
Your doctor will determine the medications to be used in a TPI.
These are usually either one or a combination of the following:
- A local anesthetic (such as lidocaine or bupivacaine): To block the pain receptors in the muscles
- A steroid (such as triamcinolone or dexamethasone): It controls the inflammation in the connective tissue and the muscles around the nerve.
- Botox (Botulinum toxin A): This prevents muscle contraction and interferes with the nerve signaling pathways.
- Saline
What to Expect During and After Trigger Point Injections?
The trigger point injection is performed in the health care professional's office. The exact technique varies but here is what you can generally expect.
Before the Procedure
Before starting, your doctor will explain the risks and benefits of trigger point injections (we will discuss that below). You may even be asked to fill out a written consent before the procedure.
Depending upon the location of the trigger point, you may be instructed to either lie on the exam table on the stomach or sit. The skin overlying the area will be cleaned with an alcohol pad (or other skin cleansers such as betadine), resulting in a cooling sensation.
Sometimes healthcare providers may mark each trigger point with a retracted pen tip or a skin marker to act as a guide before starting the procedure.
Additionally, providers may use a numbing spray (containing ethyl chloride) to anesthetize the trigger points and to make the actual injection less painful.
During the Procedure
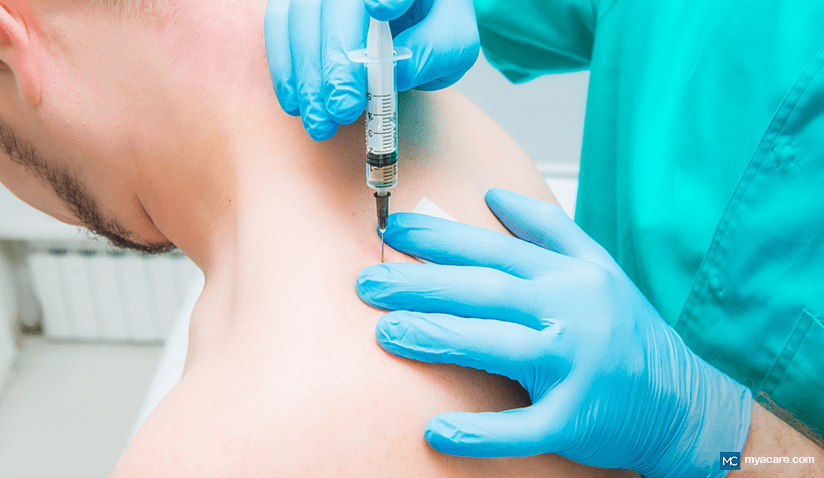
During the procedure, your doctor will press on your muscle to locate the area where you have pain. They will then use a small needle to inject medications into the trigger point.
Providers will rhythmically continue needling the area by repeatedly inserting and retracting the needle without completely withdrawing the needle from the muscle.
If you have especially tense muscles, you may feel a crunching sensation when the doctor inserts the needle. This feeling usually subsides as the muscle relaxes.
When treating multiple points, the above steps will be repeated at each site. The procedure only takes around 10 to 15 minutes.
If you have an allergy to a certain drug, a dry needle technique (without the use of medications) will be performed.
After the Procedure
Once the procedure is completed, a simple adhesive bandage may be used. Additionally, your doctor may stretch the muscle manually, applying a hot pack afterward.
If the area is painful after the injection, heat, ice, acetaminophen (Tylenol), or over-the-counter nonsteroidal anti-inflammatory medications such as ibuprofen (Advil) or naproxen sodium may be used.
If you have been given trigger point injections in your arm and legs, you will not be allowed to drive. Bring someone who can drive you home afterward.
You should avoid strenuous activity for the first few days until the muscle soreness persists. Once it subsides, begin with light stretching exercises that stretch your muscles.
You can follow this up with muscle-strengthening activities. When you can tolerate such exercises, you can gradually begin bicycling, jogging, swimming, jumping rope, tennis, etc.
How do Trigger Point Injections Work?
Trigger point injections may offer immediate benefits to people who have chronic muscle pain. Studies have shown that it can significantly improve the quality of life in people suffering from chronic pain.
Let's explore how TPI works and the scientific evidence that has studied its usefulness.
How Does it Work?
The anesthetic, anti-inflammatory drugs, and botox will allow your muscles to relax. The surrounding nerves, tissues, along with blood vessels begin to function freely again.
In the case of dry injections, the mechanism of action of trigger point injections is thought to be disruption of the trigger points by the mechanical effect of the needle.
What is the Evidence?
In a 2019 study, researchers investigated the effects of TPI in people with pain in the abdominal muscles. Two years after the initial injections, participants reported a significant reduction in pain. There were no major complications noted.
The effects of saline and lignocaine TPI were compared in the treatment of myofascial pain syndrome in a study from 2021. Researchers found that the latter showed significant improvements in pain scores, just 10 minutes after the procedure.
How Long do Trigger Point Injections Last?
The effects of TPI usually begin within a few hours. Injections containing steroids may work within two weeks.
Some people may get relief from dry injections while others do not benefit from them.
Optimally, trigger points resolve after one injection, given that you avoid the trigger.
If your pain is chronic and recurrent ( those resulting from myofascial pain syndrome or fibromyalgia), injections need to be given frequently.
The frequency of trigger point injections also depends upon the medications being injected.
If a single anesthetic drug or a mixture is used, then the injections can be administered monthly, as an ongoing therapy.
When steroid is being used in TPI, they should be administered much less frequently because of the risk of tissue damage.
What if Trigger Point Injections Don't Work?
If trigger point injections do not help relieve your chronic pain, your healthcare provider may recommend other treatments such as:
- Targeted exercises
- Stretching
- Posture changes
- Physical therapy
- Muscle relaxants
- Anti-inflammatory drugs
- Surgery
What are the Drawbacks of Trigger Point Injections?
Side effects of TPI
Some side effects associated with the procedure are:
- Bleeding.
- Pain (usually resolves by itself after a few days; more common in dry needling)
- Temporary sore or numbness after treatment
- An allergic reaction to the anesthetic medication.
- Toxicity resulting from the anesthetic medication.
- Infection.
- Swelling due to the clotting of blood within the tissues
- Injury to the blood vessels
- Dent in the skin due to shrinkage of the fat underneath (only when steroids are used)
Risks of TPI
The risk of complications from a TPI is very low. Nevertheless, some infrequent ones that have been reported in various studies are:
- Infection at the injection site
- Muscle and nerve damage
- Bruising
- Fainting
- Air enters the space between the lung and chest wall (Especially when the needle is injected into the neck and the chest) causing the lung to collapse.
- Extreme and painless muscle weakness along with paralysis.
TPI done under the guidance of ultrasound imaging can help minimize the risk of developing a serious complication.
Who Should Not Get A Trigger Point Injection?
You should avoid trigger point injections if you have any one the following:
- An ongoing infection at or over the site of the knots of muscle.
- Pregnancy.
- Taking blood-thinning medications.
- An allergic reaction to local anesthetic medications previously.
- If your doctor believes your trigger points are not safely accessible by a needle.
- Severe fibromyalgia
- You are needle-phobic and highly anxious about the procedure
- Specific mental health conditions
- Previously had a thick raised scar (keloid)
FAQS
Do trigger point injections hurt?
You may feel a stinging or burning sensation. The area may also feel a bit numb and sore for a few hours. Any discomfort is usually relieved by taking over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) or by applying heat or ice.
How much do trigger point injections cost?
The cost of a trigger point injection depends on the practitioner you choose, your location, and the number of shots you receive per session. Without insurance, the cost can vary anywhere from $250 to $450 for just the injections alone. This does not cover any extra testing that may be necessary.
What type of doctors administer trigger point injections?
Trigger point injections are frequently administered by pain-management doctors, rheumatologists, physical medicine, and rehabilitation doctors. Sometimes family practice doctors, internists, neurologists, and generalists, may also perform the procedure.
Conclusion
Trigger point injections are potential treatment options for chronic pain such as fibromyalgia, myofascial pain syndrome, and headaches. They are generally considered to be safe and minimally invasive procedures.
The procedure involves the injection of a numbing drug, anti-inflammatory medications, botox, and saline into the trigger points that can help provide pain relief. If you suffer from long-term pain, consult a trained medical professional to see if the procedure is right for your condition.
To search for the best doctors and healthcare providers worldwide, please use the Mya Care search engine.
The Mya Care Editorial Team comprises medical doctors and qualified professionals with a background in healthcare, dedicated to delivering trustworthy, evidence-based health content.
Our team draws on authoritative sources, including systematic reviews published in top-tier medical journals, the latest academic and professional books by renowned experts, and official guidelines from authoritative global health organizations. This rigorous process ensures every article reflects current medical standards and is regularly updated to include the latest healthcare insights.

Dr. Sony Sherpa completed her MBBS at Guangzhou Medical University, China. She is a resident doctor, researcher, and medical writer who believes in the importance of accessible, quality healthcare for everyone. Her work in the healthcare field is focused on improving the well-being of individuals and communities, ensuring they receive the necessary care and support for a healthy and fulfilling life.
Featured Blogs



