Non-Epileptic Seizures – Types, Causes, Symptoms, Treatments

Medically Reviewed by Dr. Sony Sherpa, (MBBS) - June 13, 2023
Difference between Epileptic and Non-Epileptic Seizures
Non-Epileptic Seizure Warning Signs
Causes - Non-Epileptic Seizures
Seizures are often associated with epilepsy, a neurological disorder characterized by recurring seizures. However, not all seizures are epileptic. Non-epileptic seizures, or psychogenic non-epileptic seizures (PNES), are a unique class of seizures that resemble epileptic seizures but are not brought on by aberrant electrical activity in the brain. These seizures can be perplexing and often require a comprehensive understanding to accurately diagnose and treat.
While epilepsy is primarily characterized by abnormal brain activity, non-epileptic seizures have psychological origins. They are thought to be influenced by emotional or psychological factors, often stemming from underlying mental health conditions or traumatic experiences.
Non-epileptic seizures are sometimes referred to as "pseudo seizures" or "dissociative seizures" because they mimic the symptoms of epileptic seizures without the presence of abnormal brain activity. The term “pseudo seizures” is, however, considered outdated since non-epileptic seizures are real and not voluntarily produced. Distinguishing between epileptic and non-epileptic seizures is crucial for appropriate diagnosis and treatment. This article will review the various types, causes, symptoms, and available treatments for non-epileptic seizures.
Difference between Epileptic and Non-Epileptic Seizures
So, what is the difference between seizures and epilepsy? Seizures can manifest in various forms and have different underlying causes. Understanding the distinction between epileptic and non-epileptic seizures is essential for accurate diagnosis, appropriate treatment, and better management of these conditions. Here are some key differences between epileptic and non-epileptic seizures:
Electrical Activity in the Brain
Epileptic seizures are characterized by abnormal electrical activity in the brain. This abnormal activity results from the excessive and synchronous firing of neurons. In contrast, non-epileptic seizures do not show any abnormal electrical activity during an electroencephalogram (EEG) test. Instead, they are thought to arise from psychological or emotional factors.
Underlying Cause
Epileptic seizures are primarily caused by disturbances in the brain's electrical activity. This can result from various factors, including genetic predisposition, brain injuries, tumors, infections, or imbalances in neurotransmitters. On the other hand, non-epileptic seizures have psychological origins. They are often associated with underlying psychological conditions, unresolved trauma, significant life stressors, or the need for coping mechanisms.
Response to Medication
Epileptic seizures typically respond to anti-seizure medications, also known as antiepileptic drugs (AEDs). These medications work by regulating the electrical activity in the brain and reducing the frequency and intensity of seizures. In contrast, non-epileptic seizures do not show significant improvement with anti-seizure medications because they do not arise from abnormal brain activity. The primary focus of treatment for non-epileptic seizures is addressing the underlying psychological factors.
Presence of Trigger Factors
Epileptic seizures can be triggered by various factors, such as sleep deprivation, stress, flickering lights, or specific medications. These triggers can vary among individuals with epilepsy and are often identifiable. Non-epileptic seizures, on the other hand, may also have triggers, but they are more closely associated with emotional or psychological factors, such as stress, trauma reminders, or intense emotional experiences.
Response to Rescue Medications
During an epileptic seizure, the administration of rescue medications, such as benzodiazepines like diazepam or lorazepam, can help terminate the seizure or prevent it from escalating. These medications act quickly on the brain to suppress seizure activity. In contrast, rescue medications are not effective in stopping non-epileptic seizures since they do not arise from abnormal electrical activity in the brain.
Psychological Assessment
Distinguishing between epileptic and non-epileptic seizures often requires a comprehensive psychological assessment. Psychological evaluations, including interviews and psychological testing, are essential in diagnosing non-epileptic seizures and identifying the specific psychological factors contributing to the seizures.
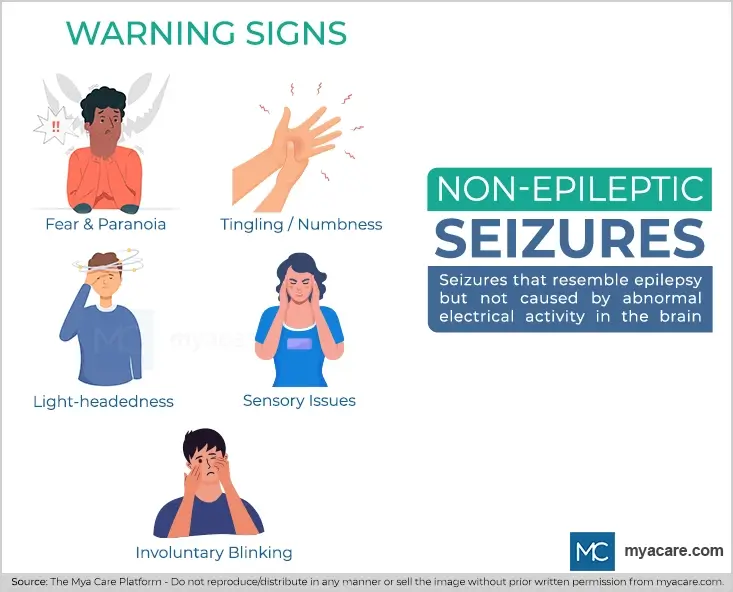
Non-Epileptic Seizure Warning Signs
Early signs of non-epileptic seizures tend to vary. Therefore, it is advisable to maintain a symptom diary to record cognitive, emotional, behavioral, and bodily signs (actual and suspected) that present prior to a seizure. Studies indicate that the following warnings signs can occur in the prodromal (early) stage:
- A sense of foreboding regarding an impending seizure and negative emotions, such as fear and paranoia
- Bodily symptoms, such as paresthesia (pins and needles sensation), numbness, fast breathing
- Sensory issues, such as impaired vision and unusual smells
- Change in consciousness, such as feeling light-headed
- Unusual behaviors, such as involuntary eye blinking
Causes of Non-Epileptic Seizures
Understanding what causes non-epileptic seizures is vital for accurate diagnosis and appropriate management. Some known causes are:
Psychological Factors
Non-epileptic seizures are often stress-induced seizures associated with underlying psychological distress. Individuals experiencing these seizures may have unresolved trauma, significant life stressors, or the need for coping mechanisms. The seizures may serve as a physical expression of emotional or psychological struggles. Common psychological factors associated with non-epileptic seizures include depression, somatization disorder, PTSD, and anxiety disorders.
Trauma
Previous traumatic experiences, such as physical or sexual abuse, combat exposure, accidents, or witnessing distressing events, can contribute to the development of non-epileptic seizures. The seizures may serve as a way for the individual to unconsciously cope with or express the emotional impact of the trauma.
Somatization Disorder
Some individuals with non-epileptic seizures may have somatization disorder, a condition characterized by the manifestation of physical symptoms without an identifiable medical cause. The seizures in these cases can be seen as a form of somatization, where emotional distress is converted into physical symptoms.
Coexistence of Epilepsy and Non-Epileptic Seizures
In some cases, individuals may have both epilepsy and non-epileptic seizures. This could complicate both diagnosis and treatment as the two conditions need to be differentiated and managed separately. The presence of epilepsy does not exclude the possibility of non-epileptic seizures and vice versa.
Symptoms of Non-Epileptic Seizures
Non-epileptic seizure symptoms can resemble those of epilepsy, making it challenging to differentiate between the two without proper medical evaluation. Non-epileptic seizures can be triggered by emotional or psychological factors, such as stress, anxiety, or intense emotional experiences. The seizures may occur during or shortly after exposure to these triggers.
Unlike epileptic seizures, non-epileptic seizures typically do not have a postictal period, which is the recovery phase characterized by confusion, disorientation, and fatigue that follows an epileptic seizure. Instead, individuals may quickly regain full consciousness after a non-epileptic seizure.
Some common symptoms of non-epileptic seizures include:
- Loss of Consciousness
- Stiffening or jerking of limbs
- Uncontrolled movements
- Convulsions resembling epileptic seizures
- Sensory symptoms such as hallucinations, numbness or tingling sensations, or changes in vision or hearing.[5]
Conditions that Mimic Seizures
Seizures can present with a wide range of symptoms, and in some cases, certain medical conditions can mimic the characteristics of a seizure. When diagnosing those who seem to have seizures but do not exhibit abnormal brain electrical activity, it is crucial to take these circumstances into account. Here are some conditions that can mimic seizures:
Syncope
During syncope episodes, individuals may exhibit muscle jerking, convulsive movements, or stiffening, which can be mistaken for a seizure. However, unlike seizures, syncope is not caused by abnormal brain activity but rather by cardiovascular or neurological factors.
Migraine
Certain types of migraines, particularly hemiplegic or complex migraines, can present with neurological symptoms that resemble seizures. These symptoms may include visual disturbances, tingling or numbness, speech difficulties, or transient weakness on one side of the body.
Transient Ischemic Attack (TIA)
Transient ischemic attacks can mimic seizures and result in sudden confusion, slurred speech, and lack of coordination. Weakness or numbness on one side of the body is another possible symptom.
Movement Disorders
Certain movement disorders, such as dystonia, chorea, or myoclonus, can result in abnormal and involuntary movements that may be mistaken for seizures. These movements can vary in intensity and duration, and a thorough examination by a neurologist can help differentiate between these movement disorders and epileptic seizures.
Sleep disorders, such as sleepwalking, night terrors, or rapid eye movement (REM) sleep behavior disorder, can involve movements, vocalizations, or behaviors that resemble seizures.
Treatment for Non-Epileptic Seizures
The management of non-epileptic seizures requires a multidisciplinary approach involving both medical and psychological interventions. Addressing the underlying psychological or emotional factors contributing to seizures is the primary goal of the treatment. Some common approaches to managing non-epileptic seizures include:
Psychotherapy
Psychotherapy, particularly cognitive-behavioral therapy (CBT), is often recommended to individuals with non-epileptic seizures. Therapy can help identify and address the emotional triggers and underlying psychological issues associated with the seizures. Techniques such as relaxation training, stress management, and coping strategies are often incorporated into the treatment plan.
Medications
There is no specific medication to treat non-epileptic seizures themselves; however, medications may be prescribed to manage any comorbid conditions, such as anxiety or depression. These medications aim to alleviate the psychological symptoms that may contribute to seizures. However, it is vital to be wary of the use of medication in treatment. Since PNES is often misdiagnosed as epilepsy or when a differential diagnosis is not possible, the treatment might include medications for seizures, i.e., Benzodiazepines. These medications suppress the respiratory system over a period of time and may cause respiratory failure in patients with PNES.
Education and Support
Providing education about non-epileptic seizures to the individual, their family, and their social support network is essential. Understanding the condition and its psychological origins can help reduce stigma, improve communication, and promote a supportive environment for the individual. Support groups and counseling services can also offer a valuable source of emotional support and guidance.
Stress Management Techniques
Deep breathing techniques, meditation, yoga, and regular exercise can help lower stress levels and improve general well-being. Such techniques address a significant trigger - stress - and can be beneficial for treatment.
Psychological Evaluation and Treatment
A comprehensive psychological evaluation is crucial in identifying any underlying psychological conditions or unresolved trauma that may be contributing to the seizures. Once identified, appropriate psychological treatments, such as trauma-focused therapy or specialized therapies for anxiety or depression, can be implemented.
Collaboration between Specialists
The management of non-epileptic seizures often requires collaboration between neurologists, psychiatrists, psychologists, and other healthcare professionals. This interdisciplinary approach ensures comprehensive assessment, accurate diagnosis, and tailored treatment plans for individuals with non-epileptic seizures.
Response to treatment for non-epileptic seizures can vary among individuals. Some may experience a significant reduction in seizure frequency or complete resolution, while others may require ongoing management and support. Patience, persistence, and a supportive treatment team are essential elements in achieving the best possible outcome.
FAQs on Seizures and Stress
Can stress cause seizures?
Yes, stress can be a trigger for seizures in some individuals. Stress can contribute to changes in brain activity and neurotransmitter imbalances, which may increase the likelihood of seizures occurring.
Can panic attacks cause seizures?
While panic attacks can be distressing and share some similar symptoms with seizures, they do not directly cause seizures. However, intense panic attacks can lead to hyperventilation, which may decrease carbon dioxide levels and potentially trigger a seizure in individuals with a preexisting seizure disorder.
What causes seizures in adults with no history of the condition?
Adults with no prior history of seizures may experience them for a variety of reasons, including head trauma, brain tumors, infections, drug or alcohol withdrawal, metabolic imbalances, strokes, and certain medical conditions like high blood pressure or diabetes.
Can heart problems cause seizures?
Heart problems can potentially cause seizures, although it is relatively rare. When the heart does not pump enough oxygen-rich blood, the blood flow to the brain might get interrupted, leading to a lack of oxygen and a subsequent seizure.
Can POTS Cause Non-Epileptic Seizures?
Postural Orthostatic Tachycardia Syndrome (POTS) is a condition characterized by an abnormal increase in heart rate upon standing. While POTS itself does not directly cause non-epileptic seizures, individuals with POTS may experience symptoms that overlap with those seen in non-epileptic seizures. These symptoms can include lightheadedness, fainting, and loss of consciousness. It is important to differentiate between POTS-related symptoms and true non-epileptic seizures to ensure appropriate management and treatment.
The Takeaway
Non-epileptic seizures, also known as psychogenic non-epileptic seizures (PNES), are distinct from epileptic seizures and have psychological origins. Although they frequently mimic epileptic seizure symptoms, they do not involve abnormal brain electrical activity. Accurate diagnosis and effective treatment depend on knowing the distinction between epileptic and non-epileptic seizures
Treatment for non-epileptic seizures involves a multidisciplinary approach, including psychotherapy, medications for comorbid conditions, stress management techniques, and collaboration between specialists. Those who experience non-epileptic seizures can lead better lives with greater seizure control by addressing the psychological issues at the root of their condition and receiving the right care.
To search for the best Neurology Healthcare Providers in Croatia, Germany, India, Malaysia, Spain, Thailand, Turkey, the UAE, UK and the USA, please use the Mya Care search engine.
To search for the best doctors and healthcare providers worldwide, please use the Mya Care search engine.
The Mya Care Editorial Team comprises medical doctors and qualified professionals with a background in healthcare, dedicated to delivering trustworthy, evidence-based health content.
Our team draws on authoritative sources, including systematic reviews published in top-tier medical journals, the latest academic and professional books by renowned experts, and official guidelines from authoritative global health organizations. This rigorous process ensures every article reflects current medical standards and is regularly updated to include the latest healthcare insights.

Dr. Sony Sherpa completed her MBBS at Guangzhou Medical University, China. She is a resident doctor, researcher, and medical writer who believes in the importance of accessible, quality healthcare for everyone. Her work in the healthcare field is focused on improving the well-being of individuals and communities, ensuring they receive the necessary care and support for a healthy and fulfilling life.
References:
Featured Blogs



