Posterior Tibial Tendinitis: Symptoms, Diagnosis, and Treatment

As we age, our bodies have a more challenging time bouncing back from strenuous activities, rigorous exercises, and high-impact sports.
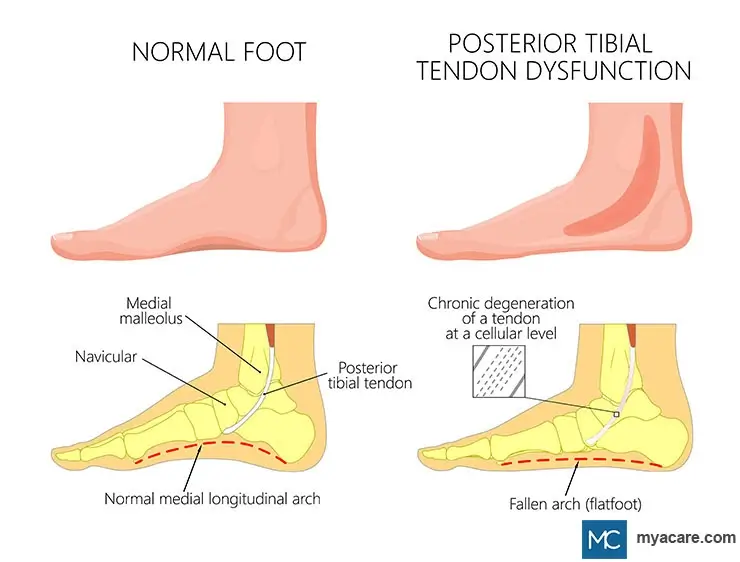
Posterior Tibial Tendinitis is an inflammatory condition commonly caused by an overuse injury or the wear and tear of aging. It’s a progressive disorder that results in debilitating pain, affecting your movement and eventually leading to flatfoot deformity.
Early diagnosis and intervention are essential to prevent its progression. Early stages of posterior tibialis tendinitis usually resolve with non-surgical treatment. But, without treatment, posterior tibialis tendon dysfunction will continue to worsen and lead to severe complications that need surgical treatment.
Read on to learn more about the symptoms, diagnosis, and treatment of Posterior Tibial Tendinitis.
What Is Posterior Tibial Tendinitis?
Posterior tibial tendonitis, also called posterior tibialis tendon dysfunction (PTTD) or tendinopathy, is the inflammation of the posterior tibialis tendon in your ankle.
The posterior tibial tendon is a major tendon of your leg, connecting your calf muscle to the bones in your foot (from the back side).
Tibialis posterior tendinopathy is primarily caused by an overuse injury or a tear in the tendon at the inner part of your ankle, resulting in pain around your ankle. It’s also caused by gradual wear and tear, making it a common tendinopathy among the aging population.
The function of your tibialis posterior tendon is to support your foot and hold up its arch. A tear or inflammation in your tibialis posterior tendon impairs the support to your ankle and can also collapse the arch of your foot, resulting in a flat foot.
What Are The Symptoms Of Posterior Tibialis Tendon Dysfunction?
Diagnosing PTTD early on is crucial in determining the proper treatment and preventing severe complications from arising.
Here are a few of the symptoms of tibialis posterior tendinopathy you need to watch out for:
- Crepitus - a creaking feeling when you move the affected tendon
- Pain in the arch of your foot
- Flatfoot deformity
- Shaky balance or gait
- Swelling along the inside of your foot or ankle
When To See Your Doctor
If you notice any of the signs of posterior tibial tendonitis, reach out to your medical practitioner when you have the chance. If you leave PTTD untreated, the pressure on your ankle and foot bones may lead to arthritis of the foot.
Early diagnosis and treatment are also crucial in preventing posterior tibial tendinitis from progressing into a tendon tear, which will probably require surgical treatment.
How Does Tibialis Posterior Tendinopathy Happen?
The posterior tibial tendons attach your calf muscles to the bones in your foot. They play a significant role in maintaining your balance and aiding in movement.
As you age, your posterior tibial tendons are affected by daily wear and tear. The collagen fibers comprising your tendons will gradually break down, weaken, and lead to painful inflammation.
Typically, posterior tendon dysfunction is caused by an overuse injury. Its location on the inside of your ankle places a significant amount of tension with repetitive movements, like running. The constant and frequent strain on your posterior tibial tendon results in inflammation and, if left untreated, even foot deformity.
Athletes active on their feet, such as runners and sprinters, are most susceptible to developing posterior tibial tendonitis. Sprains and strains to your ankle are also common causes of tibialis posterior tendinopathy.
Over time, your body has also repeatedly healed from old wounds to your posterior tibial tendons. The healing process causes your tendons to thicken. This weakens your posterior tibialis tendons, making them susceptible to ruptures.
Risk Factors Of Posterior Tibial Tendinitis
Posterior tibial tendinitis can affect anyone. However, some are more likely to be affected than others because of certain risk factors:
- Women above the age of 40
- Athletes of high-impact sports, such as basketball, football, or tennis
- Hypertension
- Obesity
- Type 1 and type 2 diabetes patients
- Rheumatoid or psoriatic arthritis
- Previous ankle injuries, such as sprains and fractures
Complications Of Posterior Tendon Dysfunction
There are four stages of posterior tibial tendonitis. With each stage, your condition may progressively worsen and lead to further complications:
- Stage 1: Your posterior tibial tendon will have little to no bruising or swelling, and you may experience mild pain in your ankle.
- Stage 2: The inflammation worsens, reducing your ability to raise your heel. You’ll likely feel sharp pain with movement.
- Stage 3: Adult-acquired flatfoot deformity sets in when the soft tissues of your foot degenerate and change the alignment of your foot.
- Stage 4: Your flatfoot deformity and stiffness will extend to your ankle joint, impairing its movement and range of motion. This severe stage of posterior tibial tendinopathy can cause debilitating pain and requires surgical intervention.
When neglected, your posterior tibial tendonitis can quickly turn severe, putting you at risk of adult-acquired flatfoot or a tibial tendon rupture that requires surgical reconstruction.
How Is Posterior Tibial Tendinitis Diagnosed?
To diagnose posterior tibialis tendon dysfunction, an orthopedic surgeon reviews your medical history and performs a physical examination to assess your symptoms.
Your physical examination will involve a series of diagnostic tests to assess the stage or severity of your condition.
- Single-leg Heel Raise: You'll be required to raise your heel on a step. If you have posterior tibial tendonitis, you may have difficulty maintaining a balanced position on your ankle. If your condition has deteriorated, it is impossible to perform this exercise without intense foot pain.
- Calf Stretching: Your orthopedist will bend your foot outward, stretching your posterior tibialis muscle. If you experience any ankle pain during the process, it may be posterior tibial tendonitis.
- Resisted Inversion: For this resistive exercise, you'll need to turn the sole of your foot inward while your physician resists the movement. Pain while turning your foot may result from posterior tibial tendonitis.
- Posture assessment: Your physician may ask you to stand straight and observe your posture from the back. If a large portion of your little toe is visible, you may have developed adult-acquired flatfoot deformity.
Your orthopedist may request imaging tests for tibial tendon dysfunction for further investigation. Magnetic Resonance Imaging (MRI), Ultrasound, and Computerized Tomography (CT) Scans can view the internal structures of your foot to determine the cause and extent of your condition.
Treatment Options For Posterior Tibial Tendinitis
Conservative treatments effectively mitigate the pain and reduce the swelling associated with the early stages of posterior tibial tendonitis.
Rest
Rest is the go-to non-surgical treatment to speed up tendon healing in posterior tibial tendinitis.
You need to cut down unnecessary movement and rest your affected foot. Your physician may prescribe ankle braces, casts, or a wheelchair to limit your activity and allow your tendon to heal.
Physical Therapy (PT)
Physical therapy is excellent non-surgical management for the early stages of posterior tibial tendonitis. Your physical therapy plan will comprise rehabilitative exercise modalities with a physical therapist to strengthen the weakened calf tendon.
Cortisone Injection
Your physician may recommend corticosteroid injection therapy as a non-operative treatment for posterior tibial tendinopathy. Cortisone or steroid injections are anti-inflammatory medications to reduce the swelling and pain from posterior tibial tendonitis.
Orthotic Devices
Foot orthoses or orthotics are common for conservative treatment for posterior tibial tendonitis. Orthotic devices are shoe inserts that support your feet and improve the shape of your flatfoot. Orthotics are easily accessible, and you may even request custom-made orthoses for a better outcome of your tibial tendon dysfunction.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
Anti-inflammatory medicines, like ibuprofen, can reduce the pain and inflammation in your tendon. Medications for posterior tibial tendinitis are more suitable for the early stages.
If you have taken medication for over 4 weeks without significant improvement, approach your healthcare provider for other treatment options for posterior tibial tendinitis.
Electrotherapy
Electrotherapy is the latest heat therapy method of easing the pain and inflammation caused by posterior tibial tendonitis. It’s entirely non-invasive, using electrodes to induce heat around the affected area. The heat stimulates the circulation to your injured posterior tibial tendon to speed up tendon healing.
Acupuncture
Acupuncture is an increasingly popular non-operative management for posterior tibial tendonitis. Clinical observations have shown that acupuncture needles applied to specific acupuncture points encourage fibroblastic activity and blood flow, both essential for wound healing.
Extracorporeal Shockwave Therapy (ESWT)
Shockwave therapy for posterior tibial tendonitis releases high-energy acoustic waves directed at affected tendons to enhance the production of growth factors and boost tissue regeneration. This results in increased collagen synthesis for better and faster tendon healing.
Platelet-Rich Plasma (PRP) Therapy
PRP Therapy for posterior tibial dysfunction is a natural, regenerative treatment that uses a high concentration of your platelets. An injection of PRP around your tibialis posterior tendon can boost your natural healing process for fast and effective tendon healing.
Surgery
If diagnosis and treatment of your posterior tibialis tendon dysfunction are delayed for too long, you might need to resort to foot surgery to repair your damaged tendons.
Let’s look at the types of posterior tibialis tendon surgery that your surgeon may recommend spending on the severity of your condition.
- Tenosynovectomy: Your surgeon can surgically remove inflamed tissue, ultimately reducing any pain, bruising, and redness from posterior tibialis tendinopathy.
- Fusion: If posterior tibial tendinitis has caused any foot bones to separate at the joint, your surgeon removes the cartilage between the joints and fuses the bones back together. Pins and screws hold the bones together, making it easier to use the affected foot.
- Osteotomy: To restore bone alignment, your surgeon can perform an osteotomy, also known as bone cutting, for the surgical reconstruction of your foot bones.
- Tendon Transfer: Your orthopedic surgeon may remove tendons from your other foot to replace the damaged tibialis posterior tendon.
- Lateral Column Lengthening: Your surgeon may perform lateral column lengthening to lengthen the affected calf muscles. This procedure is excellent for preventing the recurrence of flatfoot deformity.
Outcome Of Posterior Tibial Tendonitis
It may take as long as 6 weeks to 9 months to recover from mild posterior tibial tendonitis. Patients who limit their activities, rest, and stick to their conservative treatment plans show significant improvement.
A recent clinical study reported that almost 90% of patients responded well to orthotics and physical therapy for posterior tibialis tendon dysfunction, regaining full strength after 4 months.
Severe cases of posterior tibial tendonitis will require surgical treatment, but it may take up to a year before you make a full recovery.
Frequently Asked Questions (FAQs)
Is it okay to walk with posterior tibial tendinitis?
The early stages of posterior tibial tendinitis will allow you to walk with only mild pain. However, your symptoms will worsen as your condition progresses, leading to difficulty moving the affected foot. Reduce the use of your painful foot to give the tendons enough time to heal.
Why did I get posterior tibial tendonitis?
Posterior tibial tendonitis commonly occurs because of the wear and tear that comes with aging. Women over the age of 40 are more susceptible to developing the disorder than others. Dancers and athletes might also develop posterior tibial tendonitis because of the constant strain on their ankles and feet.
What's the fastest way to heal posterior tibial tendinopathy?
When you notice the signs and symptoms of posterior tibial tendinopathy, you rest the affected foot and apply ice packs on the affected area for about 20 minutes, 4 times daily, to reduce swelling and relieve the pain.
Does a walking boot help posterior tibial tendonitis?
Yes. A walking boot comes in handy when you're trying to limit unnecessary movement. Remember that a walking boot is only meant to provide support and should not be relied on for a full recovery.
Will my posterior tibial tendonitis go away?
Yes. With proper and consistent treatment, posterior tibial tendinitis can go away, and you can regain your full strength within a few months.
To search for the best Orthopedics Healthcare Providers in Croatia, Germany, India, Malaysia, Singapore, Spain, Thailand, Turkey, Ukraine, the UAE, UK and the USA, please use the Mya Care search engine.
Dr. Mersad is a medical doctor, author, and editor based in Germany. He has managed to publish several research papers early in his career. He is passionate about spreading medical knowledge. Thus, he spends a big portion of his time writing educational articles for everyone to learn.
References:
Featured Blogs



