The Importance of Sweating: What Is Sweat and Why Do We Need It?

Medically Reviewed by Dr. Rosmy Barrios - October 01, 2024
This article is continuously updated.
Perhaps one of the most underappreciated body functions of all time would be sweating. Most people try their best not to sweat, associating it with all sorts of social stigma. Unbeknownst to many however, sweating is one of the prime homeostatic mechanisms that serves to keep us alive on a daily basis.
The following article reviews why we sweat, what sweating is made of and how sweating works. Additionally, common myths regarding sweat are discussed (and busted) below, followed by a brief summary of sweat disorders.
Why Do We Sweat?
We sweat for two main reasons:
- Thermoregulation. The primary function of sweating is temperature control. The body produces sweat as a means to cool down when overheating. When sweat makes it to the skin’s surface, it begins to evaporate which in turn cools the skin’s surface and body as a whole. The higher the heat intensity, the more sweat is produced in order to cool the system. Once the body has acclimatized, less sweat is produced for cooling purposes.[1]
- Emotional Stress. While little is understood about stress-induced sweating, it is known that acute or chronic psychological stress can cause either hyperthermia or hypothermia[2]. When an emotional event provokes hyperthermia, sweating is the net result. Emotional sweating mostly occurs in the soles and palms, however it may also affect other areas such as the face.
Additionally, sweating can be induced by any number of factors that:
- Raise metabolic output and body temperature
- Activate thermoreceptors (e.g. consuming very spicy food)
- Increase an inflammatory immune response (e.g. allergy, injury or fever)
- Promote vasodilation (e.g. menses or menopausal hot flushes)
- Induce abnormal hypothalamic thermoregulation (e.g. sleep deprivation, age-related vascular changes)
Sweating is Important for Survival
If humans didn’t sweat, we would have likely died off as a species millions of years ago. Heat above 40˚C is able to denature proteins and kill off cells. If core body temperature exceeds this amount, it can cause heat stroke and eventually lead to multiple organ failure and death.
Before a lack of sweating becomes fatal, it is known to promote the following symptoms[3]:
- Elevated heart rate and respiratory distress
- Brain swelling and/or ischemia
- Blood fluid loss, dehydration, edema and potential kidney failure
- Increased intestinal permeability, coupled with risk of infection and hemorrhage
- Compromised circulation and risk of multiple-organ ischemia
- Electrolyte abnormalities
- Hypoglycemia, metabolic acidosis (may induce a coma) and/or respiratory alkalosis
In order to avoid symptoms of over-heating, our bodies produce sweat. Unlike other animals, humans have adapted to having a large skin surface area which is able to cool down all internal compartments of the body. Thank goodness for sweat!
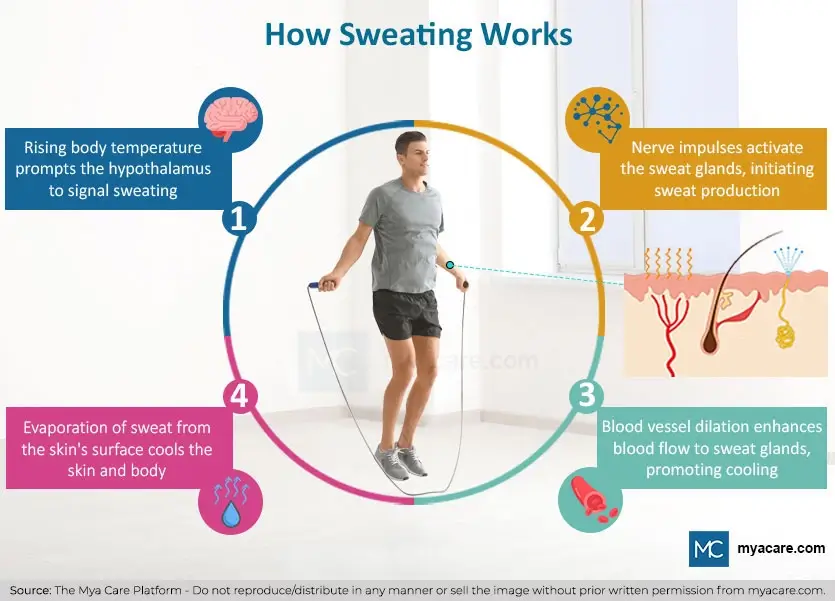
How Does Sweating Work?
Ordinary sweating is generated through the following mechanisms:
Hypothalamic Control. Sweating is governed by the hypothalamus in the brain and the autonomic nervous system throughout the body. The hypothalamus monitors the temperature of the blood, as well as nerve signals from the body to ascertain body temperature. When the body overheats, the hypothalamus sends signals to the skin to induce sweating. The hypothalamus additionally serves as a central processing unit for emotional processing, being connected to the limbic region of the brain thought to induce emotional sweating[4]. Immune signals[5], hormones, circadian perturbations and other sweat causes are also able to alert the hypothalamus to induce sweating.
Autonomic Neurotransmitters. Sweat-inducing nerve impulses are governed by both adrenergic and cholinergic neurotransmitters, however catecholamines are known to play a larger role in sweat secretion. Adrenergic innervation appears to play a larger role in emotional sweating, with greater influence on the palms and soles.
Sweat Formation. When nerve impulses reach the sweat glands in the skin, they begin to produce sweat. Sweat formation and secretion rely heavily upon sodium, chloride and calcium gradients which also govern the movement of sweat inside the gland. The gland itself resembles a knotted mass of yarn, lined with three main types of cell: myoepithelial (skin stem cells), clear cells and dark cells.
Clear cells are the main sweat producing cells, while dark cells secrete cofactors that maintain ionic balance, enhance sweat production and influence the final composition. Primary sweat secreted by these cells is an ion-rich substrate. The sweat makes its way out of the gland through the distal duct towards the skin. Along this duct, sodium and chloride ions are reabsorbed, leaving behind the final product that is sweated onto the skin’s surface.[6]
Vasodilation. During sweat onset, the hypothalamus signals for blood vessel dilation. This increases blood vessel surface area, pushes them closer to the skin’s surface for additional cooling and allows for blood fluids to quickly reach the sweat glands.
Types of Sweat Gland & Sweat Composition
Sweat glands are an extremely important component of skin that are required for its optimal functioning. It is estimated that every human contains roughly 2-5 million sweat glands.
In spite of common perceptions, sweat is largely sterile and mostly consists of salt water. The composition of sweat differs depending on the type of sweat gland that secretes it, the metabolism of the person (affected by age, gender and health status) and the conditions under which sweat is produced.
Eccrine Glands
Eccrine Glands are the main type of sweat gland found in abundance in all skin covering the body, averaging 2-4 million in total. Unlike other types of sweat glands, eccrine glands are active from birth and contribute towards cooling and skin defense. Contrary to popular belief, these sweat glands are always active, secreting a small amount of sweat all the time that often goes by unnoticed. When the body needs to cool down, their activity noticeably increases.[7]
Eccrine Sweat Composition consists mostly of water (99%) with a lesser amount of sodium chloride. Levels of salt in sweat are typically less than in blood, as the ions get absorbed before the final product is secreted onto the skin’s surface. Eccrine sweat also contains a miniscule portion of moisturizing substances, such as lactate, glucose, urea, and potassium. These enhance the effects of sebum (see sebaceous glands below) by conditioning the skin’s top layer to prevent moisture loss.
A minor fraction of eccrine sweat also contains IgA antibodies, cytokines[8], dermcidin, cathelicidin and lactoferrin, which have antimicrobial properties and serve to regulate bacteria in the skin microbiome. These substances also help to ward off skin infections.[9]
Apocrine Glands
Apocrine Glands are a secondary type of sweat gland that produces a more oily type of sweat. These are connected to hair follicles and found in body sites that typically produce an odor, such as in the armpits, breasts/pectorals, face, scalp and genital area. Apocrine glands develop in utero alongside eccrine glands, yet they only become active at puberty onset. Interestingly, emotional sweating does not appear to occur before the onset of puberty, suggesting that apocrine glands play a main role in this cause for sweat.
Apocrine Sweat Composition is very similar to eccrine sweat with the exception of containing a larger fraction of fats. Like eccrine sweat, apocrine sweat consists of an exceedingly small fraction of proteins, sugars (including lactate and glucose), steroids (hormones) and ammonia. It is believed that apocrine sweat also contains slightly more hormones than eccrine sweat. As apocrine sweat is connected to hair follicles, it blends with sebum (see sebaceous glands below) before being secreted onto the skin.
Apoeccrine Glands
Apoeccrine glands are a recently discovered sweat gland that resembles a composite of both eccrine and apocrine glands. Little is understood about this type of glands function. The bodily distribution of apoeccrine glands is similar to that of apocrine glands, and the secretions it makes are similar to that of eccrine glands. This has lead researchers to believe that it enhances the thermoregulatory properties of apocrine glands, yet more research is needed before any conclusions can be drawn.
Sebaceous Glands
Sebaceous Glands are not actually a type of sweat gland, however they contribute to the composition of sweat through the oils they secrete via hair follicles. These oils help to trap some of the water secreted by sweat glands on the skin’s surface, which in turn helps to ensure the skin remains adequately hydrated.
Aside from hydration, the oily secretions of sebaceous glands (sebum) provide a safe substrate for the skin microbiome to colonize. Sebum is known to have antimicrobial properties and promote the growth of friendly skin bacteria, which form a frontline defense against unwanted microbes in the environment.
6 Common Myths about Sweat
Most people do not appreciate just how vital sweating is for optimal health and well-being. Perceptions of sweating are often biased and not founded in fact.
The below points address some of the common misperceptions many have about sweat and elucidate what is currently known on the subject.
1. Sweating is an Important Form of Detox for Maintaining Health
Many people will advocate sweating as a means of detox for health purposes, stating that sweat is a simple method for releasing toxins from the body. Unfortunately, while it is technically accurate that sweat contains a portion of toxins, the amounts are so miniscule and obscure that sweat is not worth considering as a route of elimination.
Minimal By-Products. Sweat mostly consists of water and a small fraction of salt in the form of sodium chloride. Less than 1% of sweat contains waste products such as urea and ethanol. The concentrations of these substances in sweat are either less than or equal to that of blood and interstitial fluid (extracellular fluid separating blood vessels and other cells). In other words, when we sweat, we are mostly getting rid of extracellular water.
Exercise Enhances Liver Function. Urea excretion was proven to be much higher for exercise-induced sweating than heat-induced sweating, indicating that metabolism was the main contributing factor. [10] This result merely mirrors the elevated metabolism of the liver during exercise, which promotes an increase in urea production, blood urea concentrations and toxin elimination. By comparison to other routes of elimination, sweat still contributes minimally in this scenario. It is highly likely that sweating and exercise have been conflated in this context; with exercise and metabolism being the main means of enhanced detoxification.
Possible Heavy Metal Reduction. There are a few studies that reveal that in individuals suffering from acute exposure, concentrations of heavy metals in sweat either matched or exceeded both blood and urine levels. Sweating also appeared to top daily urinary excretion. In specific case reports, sauna-induced sweating helped to normalize blood concentrations of mercury. Additionally, sweat cadmium proved to be more concentrated than blood cadmium levels.[11]
Some sources are skeptical of these results as heavy metals are often found to contaminate the collection equipment and could contribute to false results. Other collection methods are prone to sweat evaporation, which would increase the quantity of other substances found in sweat. As the digestive tract is the main route for heavy metal excretion, these results may not accurately reflect excretion rates. Further, it ought to be noted that blood heavy metal concentrations speak very little of bioaccumulation of these toxic elements in organs and tissues. Thus, sweating is not a likely means for heavy metal detox for internal body compartments, but may aid in reducing body burden in acutely exposed individuals.
Sweat Does Not Detox a Hangover. Ethanol is another miniscule toxic by-product found in sweat in negligible concentrations. Many people believe that sweating helps to get rid of a hangover by detoxing ethanol. While the concentration of ethanol in sweat rises after alcohol consumption, it merely emulates the levels found in the bloodstream. Sweat rate does not increase after alcohol consumption and the main route of elimination still resides in the liver and kidneys. Exercise can potentially help to speed through a hangover by enhancing liver metabolism of ethanol, however it has little to do with working up a sweat.[12]
Diminishing Substance Return. Metabolism and heat acclimation both serve to promote a diminishing return with regard to substances secreted in sweat. Studies reveal that the first round of sweat typically yields larger (miniscule) concentrations of sodium and other substances in sweat, in tandem with metabolic increases and temperature acclimatization. As more sweat is produced, it becomes more and more watered down, the metabolism stabilizes and the body then adjusts to the heat. Once adjusted, less sweat is produced overall, alongside less waste products.
In conclusion, sweating does not detoxify the body, however it may contribute towards temporarily reducing a fraction of toxins from the blood.
2. When We Sweat, We Recycle Body Fluids
It may be that recycling our internal fluids is beneficial for health from the perspective that water is a prime substrate for chemical reactions in our cells and through time, it becomes altered at the molecular level. Nonetheless, research in this field is highly limited and results suggest that sweat contributes minimally towards fluid recycling as compared to other means of elimination.
Intracellular Water Excretion. According to studies, water first passes into blood and interstitial (extracellular) spaces as it makes its way down the digestive tract. Once in the bloodstream, water quickly hydrates well-perfused body compartments, including the skin, kidneys, brain, liver and spleen. However, by comparison to the water found in extracellular spaces, intracellular water takes a much longer time to turnover inside the cells of internal organs, averaging approximately 50 days from available data. Therefore, sweating is not a means for recycling internal body fluids and the kidneys are still the major route of elimination for total body water.[13]
Extracellular Water Excretion. The skin appears to maintain its own water supply for cooling purposes. Extracellular water stored in skin is converted into sweat as required; the stores of which are depleted via sweating and rapidly renewed post water ingestion. Studies show that ingested water takes about 3-10mins to reach the skin’s surface in the form of sweat in a hot environment or during exercise[14] [15]. Other than this, sweat is not known to excrete extracellular water found in other body compartments.
3. Excessive Sweat Promotes Mineral Imbalances
Exercise-induced sweating is also able to increase mineral losses to a minor degree, however these losses are most often negligible. The main minerals lost during sweating would be sodium and chloride, which account for less than 1% of sweat. Provided one is adequately hydrated, sodium loss is greater at the start of sweat onset and diminishes the more one sweats. This is in line with metabolism and heat acclimation.[16]
Athletes and Hyponatremia. Case reports on healthy athletes and military personnel reveal that they suffer more from sodium deficiencies than the rest of the general population. Studies conducted on athletes reveal that at average sodium sweat excretion rates, sodium deficiency can occur after 4hours of intensive sweating. Nonetheless, sweat tends to convey a lesser amount of sodium the longer one sweats. Other studies highlight that it can take up to 12hours of intensive exercise before an athlete suffers from a sodium imbalance.[17]
Dehydration. Sweating in dehydrated individuals can promote an increase in sodium chloride loss via sweat.[18] However it is unclear as to whether this is related to increased sodium excretion or elevated sodium to water ratios in the sweat produced. Furthermore, studies are unclear as to how long one would need to sweat in order to cause a sodium imbalance.
Over-Hydration. Sodium imbalances can also occur in the context of over-hydration. Drinking too much water can cause electrolytes to become diluted, especially sodium and chloride. This may be related to the misconception regarding sweat and mineral imbalances, particularly in individuals who frequently make use of a sauna and potentially over-hydrate. Athletes are prone to both over-hydration as well as profuse sweating. However, aside from these extreme examples, most members of the general population do not need to worry about mineral losses via sweat, particularly as dietary intake often covers or exceeds sodium requirements[19].
Disorders of Excessive Sweat Sodium. Those with cystic fibrosis are known to excrete higher than average sodium concentrations in sweat and are prone to sodium deficiencies in hot weather or after exercise due to profuse sweating.
Faulty Readings. Often the collection method is prone to inaccurate readings of minerals as well, leaving the results open to skepticism. One of the main flaws of assessing mineral losses is that the majority of minerals found in sweat are often due to dead cell debris that contains minerals. Another prime issue would be sweat evaporation, which concentrates solutes in sweat collected. Other assessments rely on calculations based on current data, which is limited and may be inaccurate.
4. Sweat Causes Body Odor
As highlighted above, sweat mostly consists of water and a lesser degree of salt. The more we sweat, the more watered down the sweat becomes, which is indicative of lessening body odor. This is especially true of eccrine sweat glands, which are the most ubiquitous type of gland found all over the body.
Body Odor is Bacterial. In body sites associated with body odor, such as under the arms, sweat contains contributions from apocrine glands, which secrete a more oil-heavy sweat. This type of sweat also consists of a higher degree of hormones, sodium, sugars and urea than eccrine sweat; however the quantities are still so small that the sweat itself is not responsible for generating body odor. Instead, scientists have discovered that bacteria present at the skin’s surface are responsible for generating body odor through breaking down the salts, sugars, oils and urea, giving rise to extra ammonia[20] and other by-products that give off a pungent smell.
Deodorant May Increase BO. Many cosmetic products are aimed at both plugging up sweat glands and destroying the microbial ecology on the skin. This can potentially increase odor in the future as it promotes the growth of unwanted bacteria and prevents sweat from being able to condition the skin properly. In this regard, it may be best to make use of products that blend with body odor, rather than attempting to be at war with your sweat glands. Natural scents often consist of essential oils which have antimicrobial properties and are able to work synergistically with the skin while covering any unwanted odors.
5. Pheromones in Sweat Promote Physical Attraction Between Partners
It’s no secret that scent plays a role in human attraction between partners. It is the same in many animal species, due to the action of pheromones (hormones that are designed to attract mates through scent). Contrary to popular opinion, human sweat does not appear to contain pheromones, in spite of the role scent plays in human attraction.
Other studies have shown that it may be the unique collection of hormones, cytokines and other by-products that contribute to the scent of human sweat which may help to attract a partner. Blood tests reveal that many successful couples appear to have complementary hormonal and cytokine profiles. However, results are still inconclusive as to whether one can “sniff out” chemical compatibility in another’s sweat and if such minor quantities would contribute towards attraction.
6. Sweat is Unhygienic
Sweat is Sterile. On the contrary, as sweat mostly consists of salt water, it actually serves to cleanse the skin of potentially unhygienic contaminants. Additionally, all sweat glands contain cells that produce antimicrobial peptides which influence the composition of sweat as well aid in protecting the microbiome of the skin.
Sweat Glands Don’t Stop. Someone may argue that the more oily secretions in sweat are prone to oxidation and contamination from the environment, rendering apocrine sweat unhygienic. The truth is that we never actually stop sweating! Our sweat glands work non-stop to ensure our skin remains hygienic and free of pathogenic bacteria.
Skin and Viral Infections. In someone who is sweating due to a skin or viral infection, sweat may be considered as a means of transmission. This is especially true of skin infections, while less is certain with regard to viral infections. Sars-CoV-2[21], zika virus[22] and human T-cell lymphotrophic virus type I[23] are known to infect sweat glands and can potentially be transmitted via sweat. Nonetheless, research is scant as to whether infectious media in sweat would be contagious, as sweat contains a miniscule fraction of antibodies and antimicrobial substances. Furthermore the skin microbiome itself is able to protect against foreign media, with friendly microbes secreting their own antimicrobial substances.
Sweat Disorders
Three main sweat disorders exist: hyperhidrosis, hypohidrosis and anhidrosis.
Causes for sweat disorders are believed to stem from nervous system dysfunction[24], shrunken or enlarged sweat glands and/or abnormal clear cell sweat secretion.[25]
Hyperhidrosis
Hyperhidrosis refers to abnormally elevated sweat production, over and above that required by the body for cooling purposes. If diagnosed in the absence of an existing condition, it is referred to as primary hyperhidrosis. Secondary hyperhidrosis is more usual and arises as a result of medication use or another medical condition.
Patients exhibit symptoms of excessive sweating for 6 months or more during the day, with reduced sweating at night. Sweating may be chronic or episodic, with episodes lasting at least 7 days minimum. [26]
Conditions in which secondary hyperhidrosis is a common symptom include[27]:
- Neuroleptic malignant syndrome
- Duchenne muscular dystrophy
- King-Denborough syndrome
- Central core disease
- Serotonin syndrome
- Hyperthyroidism
- Fever
- Pregnancy
- Menopause
- Psychiatric disorders
- Dysautonomia
- Parkinson’s disease
- Diabetes
- Addison’s Disease
What Causes Excessive Sweating
Medications that may increase sweating include dopamine agonists, antipsychotics, insulin, tricyclic antidepressants, serotonin-reuptake inhibitors, opioids, and cholinesterase inhibitors.[28]:
Treatment of hyperhidrosis mostly consists of topical solutions that block skin pores and prevent sweat secretion. Many of these contain aluminum and either act as potent skin irritants or discolor the skin. In patients for which topical solutions fail to succeed, botox injections, liposuction or radiofrequency ablation are often successful treatment options for areas prone to excessive sweating. As a last resort in extreme cases, surgery is employed to either remove nerves responsible for inducing sweat or removing sweat glands in an area prone to hyperhidrosis.
Anhidrosis and Hypohidrosis
Anhidrosis refers to the inability to sweat and hypohidrosis refers to a reduced capacity to sweat in response to appropriate stimuli. Unlike hyperhidrosis, these conditions almost always occur secondary to another medical condition. Patients with an impaired sweating ability are at a greatly increased risk of heat stroke and fatality in hot environments.
Conditions in which reduced sweating and/or anhidrosis are common symptoms include:[29]
- Anhidrotic ectodermal dysplasia
- Aging
- Tattooed skin
- Diabetes
- Multiple sclerosis
- Systemic sclerosis
- Sjogren’s syndrome
- Skin wounds and burns, including sunburn
- Spinal cord injury
- Heat rash (miliaria rubra)
- Eczema, psoriasis and other obstructive skin conditions
- Genetic conditions such as Fabry’s disease
Medications that result in reduced sweating include tricyclic antidepressants, carbonic anhydrase inhibitors, calcium channel blockers, adrenergic blockers, anticholinergic agents and antimuscarinic drugs.[30]
Treatments for anhidrosis and hypohidrosis are not readily available as of yet. Patients are required to remain cool at all times and often find relief in making use of a spray bottle in hot environments. In obstructive skin conditions in which sweat glands are occluded, exfoliation is recommended.
Conclusion
Sweat is a vital body function, necessary for our survival. The primary function of sweat pertains to cooling the body down, with consequences of overheating being potentially fatal. The skin requires sweat to remain hydrated and to maintain a healthy microbial environment. Sweat mostly comprises water, with less than 1% consisting of sodium chloride and negligible amounts of various other substances. As a result, sweat is not a main route for elimination, excretion or detoxification. However prolonged periods of profuse sweating may contribute towards dehydration and sodium imbalances under rare conditions. In individuals with sweat disorders, care ought to be taken to ensure adequate thermoregulation is maintained at all times.
To search for the best doctors and healthcare providers worldwide, please use the Mya Care search engine.
The Mya Care Editorial Team comprises medical doctors and qualified professionals with a background in healthcare, dedicated to delivering trustworthy, evidence-based health content.
Our team draws on authoritative sources, including systematic reviews published in top-tier medical journals, the latest academic and professional books by renowned experts, and official guidelines from authoritative global health organizations. This rigorous process ensures every article reflects current medical standards and is regularly updated to include the latest healthcare insights.

Dr. Rosmy Barrios is an aesthetic medicine specialist with international work experience. She earned her physician diploma at the Universidad Del Norte’s School of Medicine in Barranquilla, Colombia, and her specialty at John F. Kennedy University in Buenos Aires, Argentina. Dr. Barrios is a member of the Pan-American Aesthetic Medicine Association (PASAM) and the Union Internationale de Médecine Esthétique (UIME). She is an expert health writer with keen interests in aesthetic medicine, regenerative aesthetics, anti-aging, fitness, and nutrition. Currently, Dr. Barrios heads the Regenerative Aesthetics department at a renowned Internal Medicine clinic based in Belgrade, Serbia.
Sources:
Featured Blogs



