What Is Carotid Artery Disease
Carotid arteries are large vessels located in the neck that supply blood to the brain, face, and neck. Carotid artery disease occurs when these blood vessels are narrowed or blocked due to the deposition of plaques. The plaques usually consist of fats, calcium, tissue, and cell debris. Carotid arteries clogged with plaques become stiff and have trouble delivering oxygen and essential nutrients. As carotid arteries are the primary source of oxygen to the brain, their narrowing or blockage increases the risk of depriving the brain of oxygen, resulting in a stroke. Stroke is a medical emergency and the fifth leading cause of death in the United States.
Symptoms of carotid artery disease
In the initial stages, individuals with carotid artery disease do not show any signs or symptoms. And hence, the condition usually goes unnoticed until the patient suffers a transient ischemic attack (TIA) or a stroke.
A TIA occurs when the blood flow to the brain is low or when a plaque briefly obstructs the blood flow to the brain. The symptoms of TIA are usually brief and may resolve within minutes to hours. Typical symptoms of TIA include:
- Transient numbness on one side of the face
- Temporary limb weakness, also usually in one side of the body
- Brief trouble in seeing
- Momentary loss of balance as well as dizziness
- Brief confusion and disruption in speech
TIA is also a medical emergency because it may lead to a major stroke. Stroke, which causes a more severe disability, occurs when a carotid artery becomes so narrow due to the plaque buildup that enough blood does not reach the brain. The more significant the narrowing of the carotid artery, the more concerning the disease is. Plaques are also prone to breakage. A stroke can also happen when a small piece of plaque breaks from the carotid artery and blocks any downstream smaller blood vessels (originating from the carotid arteries) in the brain. The disability that occurs from stroke depends on the affected brain region. Symptoms of a stroke are similar to the ones seen in TIA and may include the following:
- Sudden loss of vision in one or both eyes
- Weakness in half of the body
- Paralysis or failure of locomotor function
- Sudden confusion
- Dizziness
- Difficulty in speaking and processing language
- Sudden extreme headache
- Difficulty in memory processing
- Difficulty in swallowing
Further, sometimes, the breakage of plaques injures the blood vessels, leading to blood clots in these vessels. This can cause significant and permanent damage to the brain tissue, making a deadly disease even more lethal.
At-Risk population
Certain pre-existing conditions or unhealthy diets/lifestyles that cause plaque buildup in the blood vessels can put an individual at risk of developing carotid artery disease or related complications. Generally, the following conditions are classified as risk factors for carotid artery disease:
- Hypertension or high blood pressure
- Chronic smoking
- Diabetes
- Coronary artery disease
- Family history of stroke, coronary artery disease, or peripheral vascular disease
- Obesity
- Elevated fats in the blood or hyperlipidemia
- Sedentary lifestyle or lack of exercise
- Advancing age
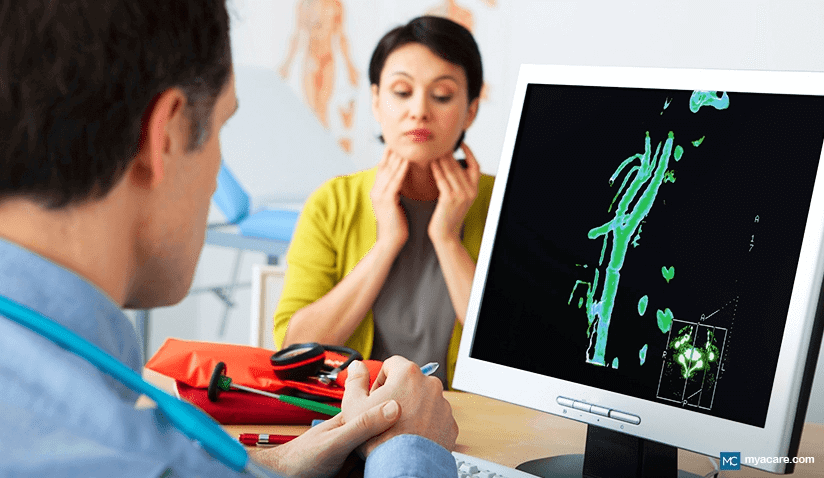
Diagnosis of carotid artery disease
Most individuals with carotid artery disease do not have any clinical symptoms. When such patients go for a regular physical exam, the primary care physician can identify the first signs of carotid artery disease. Usually, carotid artery disease is suspected during a physical exam if the doctor finds a specific noise or bruit in the neck area. These patients are then sent for further imaging tests to evaluate the carotid arteries. The most commonly used imaging techniques to rule out carotid artery disease are carotid ultrasound, magnetic resonance angiography, computerized tomography angiography, and cerebral angiography. The following table depicts the significant differences between these imaging techniques:
|
|
|
|
|
|
|
|
|
|
|
Uses high-frequency sound waves to visualize carotid arteries |
Uses powerful magnets to generate high-quality images of the brain and carotid arteries |
Uses low levels of radiation to collect pictures of the brain and carotid arteries |
A doctor visualizes carotid arteries in real-time by injecting a dye directly into the carotid arteries and monitoring them on a live X-ray screen |
|
Generally used for initial diagnosis |
Generally used to ascertain the extent of damage that has occurred in the brain due to carotid artery disease |
Can be used interchangeably with magnetic resonance angiography depending upon its availability |
Most sensitive and specific test in diagnosing carotid artery disease since the provider is accurately able to visualize the vessels in real-time |
The doctor evaluates the degree of carotid artery blockage during the diagnostic process. The disease is considered mild if the blockage is less than 50%. A moderate blockage is from 50-69%. The condition is deemed severe if a significant amount of the artery is blocked, i.e., more than 70%.
Treatment of carotid artery disease
Treatment of carotid artery disease involves a two-pronged attack. One is to prevent more blockages from forming, and the second is to treat existing blockages. The healthcare provider designs the treatment regimen for individual patients according to their age, disease severity, family history, and tolerance to specific procedures. The initial step is to start with lifestyle modifications and medications to prevent further damage. If the blockage is significant, surgical or interventional strategies are pursued to remove the plaque or open the blocked carotid artery through stent placements.
Lifestyle modifications recommended for carotid artery disease include maintaining a healthy weight through exercise and a healthy diet, limiting salt and fat intake. In general, the following changes are recommended to prevent carotid artery disease from progressing through plaque buildup:
- Regular exercising to maintain a healthy weight.
- Control diabetes and high blood pressure by eating a balanced, heart-healthy diet.
- Limit alcohol.
- Quit smoking.
- Control stress and anxiety through relaxation techniques like meditation and yoga.
- Regular follow-ups with the healthcare provider.
For mild to moderate carotid artery disease, the doctor may recommend medications that target the bad fats in the body. If the patient has a history of high blood pressure, antihypertensives are also prescribed to reduce blood pressure. Along with these medications, the doctor may also recommend using antiplatelets. These medicines prevent the formation of new clots in the blood vessels.
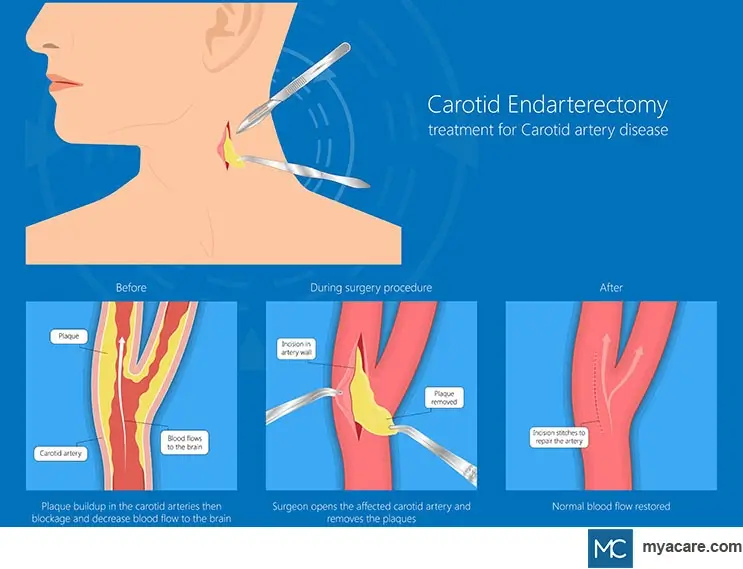
For severe carotid artery diseases, doctors recommend surgical and interventional procedures. Following are the two commonly used procedures in patients with severe carotid artery disease:
- Carotid endarterectomy is a standard procedure for carotid artery disease. It is carried out under general anesthesia. In this procedure, a small incision is made in the neck, the affected carotid artery area is cleaned, and the plaque is shelled out. As the plaque is removed, the normal blood flow to the brain is restored. This procedure requires hospitalization of 24-48 hours, and the patients can get back to their routine activities in about a week.
- Stent angioplasty is a procedure where a stent is placed in the carotid artery to open up the blocked area. A thin wire and a small balloon are guided to the blockage in the vessel through a catheter via the groin artery. The balloon is then inflated to open the blockage, and a stent is placed in the area to keep the artery open. This procedure is done under conscious sedation (a form of milder anesthesia) and hence does not require general anesthesia. Since it is less invasive as compared to carotid endarterectomy, the recovery time is much shorter.
Concluding remarks:
Carotid artery disease is a deadly condition that requires an aggressive and tailored treatment under the watchful supervision of a trained healthcare professional. Every effort should be made to prevent it by adopting a healthy lifestyle as outlined above.
To search for the best Neurology Healthcare Providers in Croatia, Germany, India, Malaysia, Spain, Thailand, Turkey, Ukraine, the UAE, UK and the USA, please use the Mya Care search engine.
To search for the best healthcare providers worldwide, please use the Mya Care search engine.
Dr. Vedangana Saini has a Ph.D. in Neuroscience. She has done multiple postdoctoral fellowships from the University of Nebraska Medical Center, Omaha, and Weill Cornell Medicine, New York. Currently, she is working as a freelance scientific writer with a mission to educate the lay public about recent scientific and medical developments. Dr. Saini has written extensively on healthcare, neuroscience, and mental health. She holds several publications in peer-reviewed journals in the form of research papers, review articles, and book chapters.
References:
Featured Blogs



