What Is Osteomyelitis?
Updated 31 August 2023
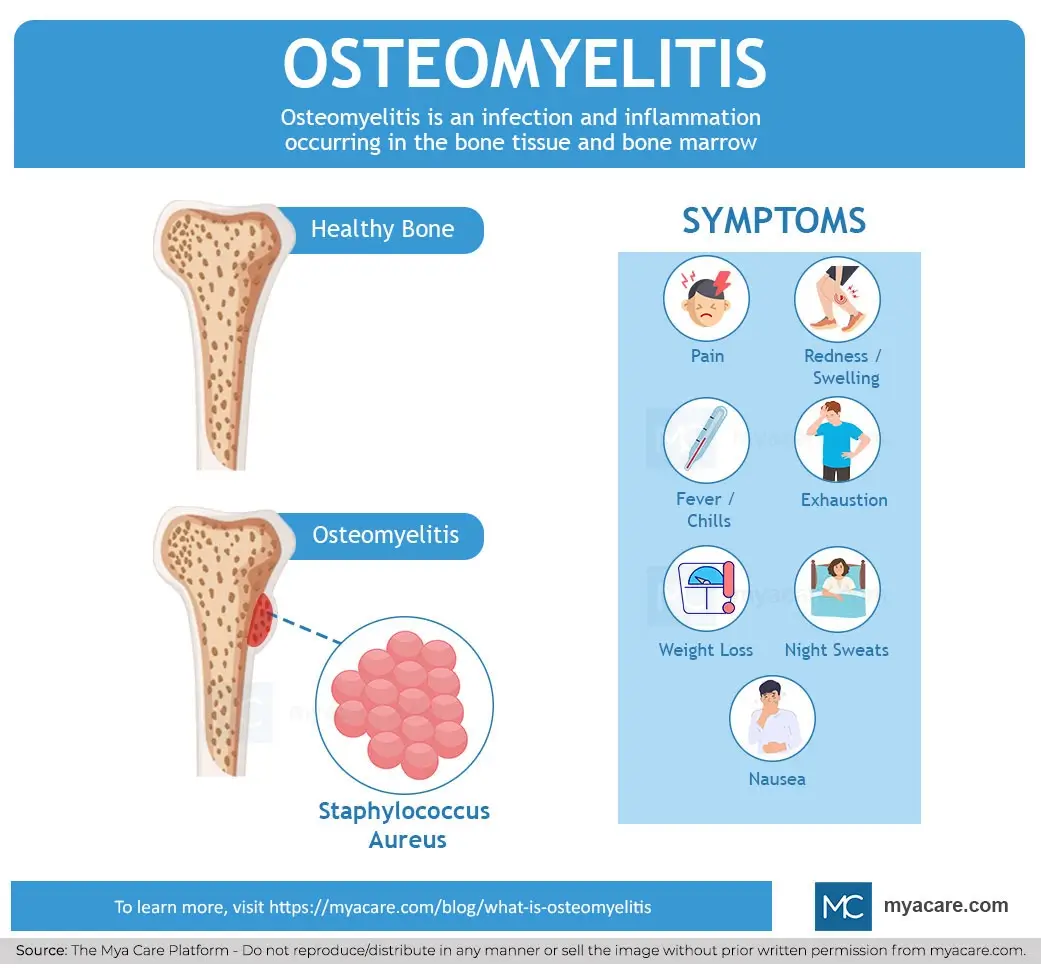
Osteomyelitis by definition is an infection and inflammation that takes place in the bone tissue and bone marrow. The infection can occur in any bone of the body and is most often due to bacterial infection. Osteomyelitis is a serious condition with a mortality rate of 1 in 5 people if treatment is not started rapidly. There are subtypes of osteomyelitis based on the cause and type of pathogen involved.
Causes of Osteomyelitis
The reasons people develop osteomyelitis are due to some infection caused by a pathogenic organism. The harmful pathogens that cause the condition may spread from a wound, a surgical site, or a prosthetic device such as an artificial joint, or through the blood from elsewhere in the body.
Dental surgery can also cause osteomyelitis of the jaw. Indwelling catheters can become infected in a healthcare setting, which can result in infections like osteomyelitis.
The bacteria implicated in causing osteomyelitis are described below:
- Staphylococcus aureus: S. aureus is the cause of the vast majority of osteomyelitis cases. This bacterial species may sometimes be resistant to methicillin antibiotics in which case it is called methicillin-resistant Staphylococcus aureus (MRSA). Antibiotic resistance is a cause for concern because it can complicate treatment and delay recovery.
- Pseudomonas aeruginosa: A species of bacteria that is commonly acquired in the hospital. Such infections that happen in a healthcare setting are known as nosocomial infections.
- Serratia marcescens: An opportunistic bacterium that is often introduced through catheters and respirators. It is also often a nosocomial infection.
Other pathogens can on occasion cause bone infections. These include the following:
- Fungi: Histoplasmosis, coccidioidomycosis, and blastomycosis can be a problem in people with a weak immune system response.
- Mycobacteria: Nontuberculous mycobacteria are those that don’t cause TB, but can infect bones.
Types of Osteomyelitis
Acute osteomyelitis is a condition where the infection spreads from the blood into the bone tissue. This is often the case with children. In adults, it is more common that the situation is one of chronic osteomyelitis. Chronic osteomyelitis is more dangerous than the acute form and harder to manage.
There are some comorbidities that are common with osteomyelitis. Discitis often occurs at the same time as osteomyelitis. Discitis is when there is an inflammation that is present between the intervertebral discs.
These discs are the pieces of cartilage found between the actual bones (vertebrae) making up the backbone. Vertebral osteomyelitis can also occur. This is when the infection is in the vertebrae.
Osteomyelitis Symptoms
The symptoms of osteomyelitis are given below.
- Pain in the affected region
- Redness and swelling of the part that is infected.
- Fever and chills
- Exhaustion
- Weight loss
- Night sweats
- Nausea
Osteomyelitis Complications
There are a couple of complications that can happen if your osteomyelitis is not treated and managed correctly. These complications are listed and described below.
- Osteonecrosis: If the bone tissue dies the bone needs to be surgically removed. This could mean limb amputation.
- Skin cancer: This is when pus from the infected bone affects the skin leading to squamous cell cancer.
- Septic arthritis: The condition when the infection disseminates into a nearby joint.
- Growth delay or impairment: In children, osteomyelitis can result in the bones not growing properly.
- Epidural abscess: This is when there is an infection between the brain and the epidural membrane.
Risk Factors for Osteomyelitis
People who have certain disorders have an increased chance of osteomyelitis. These are described below.
- Diabetes: Diabetics are much more prone to bone infections than the general population, and they are also more apt to develop the chronic form of osteomyelitis.
- Rheumatoid arthritis: This autoimmune condition makes people vulnerable because immunosuppressant medicine needs to be used, which increases susceptibility to other infections.
- HIV: The virus that causes AIDs suppresses the immune response.
- Sickle-cell disease: The odd-shaped blood cells can get stuck in blood vessels in the bones and increase the odds of infection as a result.
- Drug abuse: IV drug use makes individuals vulnerable to injecting infectious bacteria into the body.
- Alcohol abuse: Alcohol impedes bone growth and repair.
- Open wound: Any injury exposing the tissues of the body can become infected by harmful bacteria.
Osteomyelitis Diagnosis
Diagnosis is important because the infection will only become worse in time, resulting in dangerous complications.
Diagnosis of osteomyelitis is done in the following ways:
- Blood tests: Two tests are done here to test for an inflammatory response in the body. These two tests only show that inflammation is occurring and not the specific cause, so further testing is needed. The two blood tests are as follows:
- C reactive protein: This is a protein made in the liver in response to inflammation in the body.
- Erythrocyte sedimentation rate (ESR): This is a test to see the speed at which red blood cells separate from the blood plasma.
- Culture of bone tissue: A sample of tissue or fluid from the bone or marrow may be extracted and then grown in culture to identify the causative organism.
- Radiography: An X-ray of osteomyelitis or an MRI can help show abnormalities in the bone. Sometimes they use radioisotopes or other contrast material so that a defect will be visible in an imaging study.
Osteomyelitis Treatment
Treatments for Osteomyelitis include the following:
- Surgical intervention: Necrotic tissue needs to be excised to prevent gangrene from developing, which can lead to death.
- Antimicrobial therapy: Usually infections are bacterial in origin such that antibiotic use is required. The type of antibiotic used depends on if a condition is chronic or acute.
- For chronic osteomyelitis: Ampicillin/sulbactam is used intravenously.
- For acute osteomyelitis: Vancomycin or oxacillin is given intravenously.
- Antifungals may be needed where fungi such as Candia and Aspergillus infect bone tissue. However, fungal infections are rare and are more likely in people who are immunodeficient.
Conclusion
Osteomyelitis is a debilitating and dangerous condition that can result in severe consequences such as gangrene and death. The illness can be acute or chronic and it is more prevalent in people who already have underlying illnesses. Quick diagnosis and antimicrobial therapy are very important in ensuring the recovery of patients with osteomyelitis.
To search for the best Orthopedics Healthcare Providers in Croatia, Germany, India, Malaysia, Singapore, Spain, Thailand, Turkey, Ukraine, the UAE, UK and the USA, please use the Mya Care search engine.

Dr. Rae Osborn has a Ph.D. in Biology from the University of Texas at Arlington. She was a tenured Associate Professor of Biology at Northwestern State University, where she taught many courses to Pre-nursing and Pre-medical students. She has written extensively on medical conditions and healthy lifestyle topics, including nutrition. She is from South Africa but lived and taught in the United States for 18 years.
Sources:
Featured Blogs



