The Respiratory System
Medically Reviewed by Dr. Sony Sherpa (MBBS) - September 13, 2024
The respiratory tract is responsible for processing the air we breathe, in contrast to the digestive tract, which processes the solids and liquids we consume. The two tracts are similar in that they extract nutrients that our cells need in order to function.
Food alone is not enough to sustain the body’s energy requirements; rather, is a substrate of building materials that cells can use to produce complex substances. Oxygen is instead the main force driving cellular energy production – the “bio-electricity” that makes all cellular functions possible.
The functions, anatomy, and regulation of the respiratory system are discussed below, as well as the mechanisms that underpin breathing.
Functions of the Respiratory Tract
The respiratory tract serves three main functions, as follows:
- Inhalation and extraction of oxygen from air for bodily energy production.
- Elimination and exhalation of gaseous waste products.
- Protection against airborne particles.
The first function outlined above is the most important function of the respiratory system and is entirely vital for the life of all complex organisms. This is due to the fact that the body cannot sustain its high cellular energy requirements from food alone, with oxygen being a primary necessity for the continuous generation of energy.
The respiratory system also acts as an air filtration system, helping to keep potentially harmful airborne particles from entering the lungs. These include allergens, pathogens, noxious gases, and other volatile pollutants found in the air.
The lung performs several other vital functions that have little to do with respiratory function. These include[1]:
- Absorption, metabolism, and transformation of substances from both the body and the air, including inhaled medications, hormones, cellular metabolites, and more.
- Detecting and protecting against hypoxia or oxygen deprivation.
- Participating in cardiovascular system regulation by acting as a reservoir of blood. Excess blood is stored in the lungs and released into pulmonary circulation in order to help the heart during times of distress.
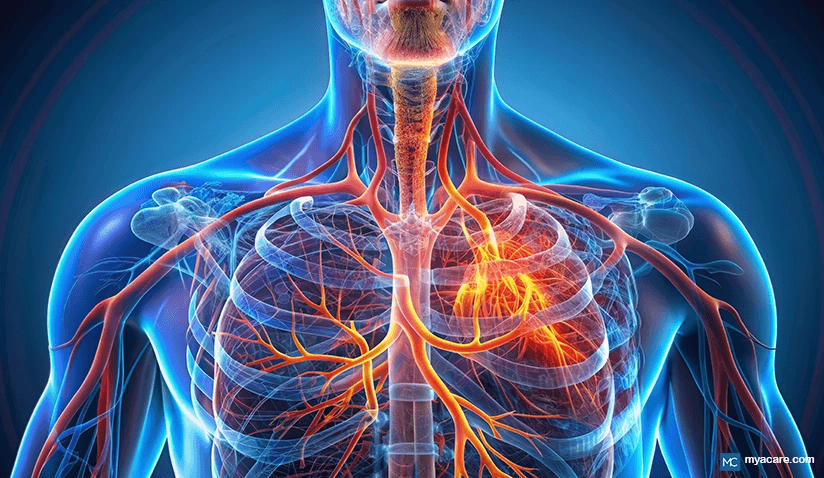
Respiratory Anatomy
The respiratory tract is divided into the upper and lower respiratory tracts.
The upper tract comprises the nose, pharynx, and larynx, while the lower tract comprises the trachea, bronchi, bronchioles, alveolar sacs, alveolar ducts, and alveoli. [2]
Additionally, the respiratory muscles accompany the respiratory tract to facilitate breathing.
Upper Respiratory Tract
The upper respiratory tract facilitates the movement of air to and from the lower respiratory tract. It also serves to protect the lungs from airborne particles.
The pharynx divides the respiratory tract from the digestive tract, with the larynx resting in front of the esophagus at the point of convergence. A muscular flap known as the epiglottis ensures that food does not enter the respiratory tract, preventing its access to the windpipe (trachea) when one eats or drinks[3].
Just like in the digestive tract, the inner nose and pharynx are lined with a mucous layer[4]. This layer acts as a filter, trapping dust and other airborne particles that are too big to cross over into the lungs. The immune system of the upper tract contributes antibodies to the mucosa in the form of secretory IgA[5]. Secretory IgA binds to foreign proteins, including allergens and some pathogens, allowing for them to be easily disposed of by the immune system. Lymph glands, such as the tonsils, house immune cells that are active in cleansing the nose and pharynx of pathogens and other hazardous materials.[6]
The nose and pharynx also house a microbiome[7], which informs the immune system of a potential danger and serves to beneficially compete with the high microbial volume in the air that we are exposed to every day. This microbiome feeds into the lungs[8], as does that of the mouth. In this respect, good nasal and oral hygiene can help to improve the health of the respiratory tract.
Lower Respiratory Tract
The lower respiratory tract facilitates the movement of air to and from the alveoli in the lungs. The trachea ends where the bronchi begin. The bronchi are the two tubes that divide the respiratory tract into the two lungs. Bronchi continue to branch off – just like a tree - into smaller and smaller bronchioles, which eventually meet with alveolar ducts. The ducts connect to sacs that house hundreds of alveoli, resembling perfectly rounded bunches of grapes. Alveoli are where the lungs absorb oxygen and eliminate carbon dioxide.
The lungs are divided into five compartments, with two being on the left and three being on the right. Each of these compartments collectively contains more than 300 million alveoli to maximize oxygenation[9], yielding a surface area of 70m² on average. Mature lungs tend to process anywhere between 10,000 to 20,000 liters of air each day!
The lower portion of the respiratory tract is intimately involved with pulmonary circulation and the cardiovascular system. Breathing sets the pace at which blood is oxygenated in the lungs and helps to regulate blood flow in the pulmonary tract. To a greater extent, this plays a role in regulating the heartbeat and vice versa, with the heartbeat regulating the way in which we breathe.
Just like the upper tract, the lower tract maintains a mucosal layer that helps to protect the lungs from particles in the air[10]. Likewise, the mucosa of the lungs also houses a microbiome[11] that protects the lungs from pathogenic colonization and alerts the immune system (via microbe-cell signaling) any moment it comes into contact with hazardous material.
Respiratory Muscles
Beneath the lungs rests the diaphragm. The diaphragm is the main respiratory muscle, with the muscles of the rib cage also playing a role in respiration.
When the diaphragm contracts, it pulls the lungs downward and increases their internal volume. This, in turn, lowers the air pressure inside the lungs and causes air to be pumped in from the external environment. When the lungs expand in this manner, the muscles of the ribcage contract and expand to give the lungs enough room to fill with air. These muscles are referred to as the intercostal muscles. Exhaling is characteristic of all muscles relaxing, requiring no effort unless air is consciously forced out of the lungs by the individual.
The diaphragm also has several other functions, including separating the chest from the abdomen and aiding in the event of crying, sneezing, coughing, hiccupping, and excretion.[12] Some scientists argue that the diaphragm consists of two muscles, with one assisting in digestive processes and the other assisting with respiration[13]; however, more evidence is required to substantiate such claims.
How Breathing Works
Respiration can be broken down into three main essential components[14]:
- Ventilation is the rhythmic or tidal movement of air in and out of the lungs, commonly referred to as breathing.
- Perfusion is the movement of blood through the lungs.
- Diffusion is the passive movement of gases (mostly O2 and CO2) across the membranes of the alveoli into the bloodstream.
All three are affected and regulated by pulmonary circulation, the breath, and the heartbeat. Ventilation (breathing) is further regulated automatically (involuntarily) by the brainstem. If any one of the above is severely compromised, it could be fatal to the organism.
Cellular diffusion of oxygen occurs in the alveolar sacs that house hundreds of alveoli. The alveoli consist of minuscule structures that specialize in absorbing oxygen from the air in exchange for carbon dioxide. Gas in the alveoli comes within 1 micrometer of that in the bloodstream to make this exchange possible in a way similar to that of osmosis.
The oxygen moves across alveolar membranes to the heme group in the hemoglobin of red blood cells, chemically binding to iron molecules to allow for adequate transport in the bloodstream. In this way, oxygen is distributed all over the body and goes on to produce energy in all our cells. Carbon dioxide binds similarly and is exchanged for oxygen as a gaseous waste product.[15]
Before the air can move across into pulmonary circulation, it needs to be conditioned for easy diffusion – a function that the lungs fulfill. When air travels into the depths of the lower respiratory tract, it is filtered, becomes warm, and is humidified, which helps to disperse molecules evenly for gaseous diffusion.[16]
The amount of air we inhale in each breath and the rate at which we breathe are both variable, often changing to suit the metabolic requirements of the body. For instance, breathing becomes more labored during exercise when there is an increase in metabolic demand and energy production. By contrast, breathing is slower during sleep when energy requirements are less.
Cardiovascular diseases are associated with the onset of respiratory ailments due to the respiratory tract’s role in the pulmonary system.[17] However, respiratory ailments are not associated with cardiovascular disease onset.
Respiratory System Regulation
The respiratory system is regulated by nearly every organ and tissue of the body as it needs to ensure that respiration on the macro level meets the O2 demands of respiration at the cellular level. This is achieved primarily via neurofeedback to the brainstem as well as modulations in blood chemistry and pressure.
Neuro Regulation
The brain and lungs have a unique relationship in regulating one another’s functions via carbon dioxide levels in the bloodstream and cerebrospinal fluid. Chemical receptors in the medulla oblongata of the brainstem, pulmonary blood vessels, and cerebrospinal fluid are able to sense the levels of carbon dioxide relative to oxygen. When the levels of CO2 are too high, the chemical receptors of the medulla are activated, and ventilation is increased through neuroendocrine feedback to the respiratory muscles.[18]
Smoking, exercising, and prolonged periods of hampered breathing can cause a rise in CO2 blood levels sufficient to increase one’s respiratory ventilation rate. If one gets stressed, experiences love, or has any other similar emotional reaction in response to environmental cues, higher centers of the brain are involved in promoting increases or decreases in ventilation.[19]
Sensory receptors also exist in the lungs that alert the brain of excessive compression, a lack of internal air pressure, and other similar compromises to breathing. These receptors are usually involved in producing hyperventilation and coughing responses from the lungs.[20]
Blood pH
Blood pH is maintained by the balance of H+ and HCO3- (bicarbonate) ions, which is maintained via the respiratory system and kidney elimination. In blood vessels, CO2 is transformed into carbonic acid, which is further broken down into HCO3- and H+ ions. This transformation can occur both ways, allowing for the respiratory system to compensate for high or low body acidity by increasing or decreasing the amount of CO2 expired with every exhalation.[21] As a result of neuroendocrine feedback mechanisms, blood pH directly regulates the actions of the respiratory system.
The digestive system, kidneys, and brain[22] are indirectly capable of regulating respiratory function via blood pH. The digestive system is constantly using up bicarbonate in order to balance the acidity of digestive juices, often relying on respiratory and pulmonary input the moment this balance is off. The kidneys are responsible for the uptake and elimination of acids and bases, and also rely on help from the lungs when they are overburdened.
Pulmonary Circulation
The blood flow to the respiratory system is largely regulated by pulmonary circulation. Unlike other organs of the body, the blood vessels of the lungs remain relaxed at all times to allow for gaseous diffusion. The only thing that regulates blood flow into the lungs is the beating of the heart. Breathing slows or speeds up in tandem with our heartbeat, both of which are neurologically regulated in the brain stem.
The pulmonary blood vessels of the lungs are, in turn, regulated by breathing itself. When the pressure in the blood vessels is too low versus the air pressure found in the alveoli, blood flow stops, and gases are exchanged. When the pressure in the blood vessels is higher, the blood is allowed to flow through again to make way for more oxygen to enter circulation and more CO2 to exit. [23]
The Respiratory Microbiome
It has recently been discovered that just like the digestive tract, the respiratory tract houses a microbiome of its own. The air we breathe contains approximately 10^4-10^6 bacteria per cubic meter. The upper respiratory tract is exposed to a lot more bacteria every day and, as would be expected, contains a much higher density of bacteria than the lower tract.[24] [25]
As seen in the gut microbiome, respiratory microbes interact with the immune system present in the lungs, regulating its actions. Probiotic bacteria communicate via cell signals that inform the immune system of a threat and also perform functions that aid in stabilizing the environment. As our understanding of the respiratory microbiome is in its infancy, it is suspected that it influences and regulates respiratory function to a greater extent than we currently understand.
Lung diseases have been associated with a lung microbiome that is out of balance (known as dysbiosis), which typically indicates a lack of probiotic diversity in which either one or a few healthy strains dominate and/or pathogenic colonization. [26] Respiratory health, on the other hand, is characterized by the presence of a healthy microbial community residing in the respiratory tract.[27]
Respiratory microbe imbalances are also linked to gastroesophageal reflux as well as increased micro-aspiration, in which trace amounts of food, saliva, and other inappropriate material make their way down the windpipe[28]. Gastric reflux is a common cause, creating an overly acidic environment in the lungs that promotes the growth of pathogenic organisms.
In small amounts, micro-aspiration helps to keep the lung microbiome healthy; however, in larger amounts, on a consistent basis, the respiratory microbiome can become unbalanced, leading to chronic inflammation and gradually impaired respiratory function[29] [30]. Healthy lung microbiomes are associated with better lung function and less arterial stiffness in aging populations.[31]
To search for the best Pulmonary and Respiratory Medicine healthcare providers in Germany, India, Malaysia, Spain, Thailand, Turkey, the UAE, the UK and The USA, please use the Mya Care Search engine
To search for the best healthcare providers worldwide, please use the Mya Care search engine.
The Mya Care Editorial Team comprises medical doctors and qualified professionals with a background in healthcare, dedicated to delivering trustworthy, evidence-based health content.
Our team draws on authoritative sources, including systematic reviews published in top-tier medical journals, the latest academic and professional books by renowned experts, and official guidelines from authoritative global health organizations. This rigorous process ensures every article reflects current medical standards and is regularly updated to include the latest healthcare insights.

Dr. Sony Sherpa completed her MBBS at Guangzhou Medical University, China. She is a resident doctor, researcher, and medical writer who believes in the importance of accessible, quality healthcare for everyone. Her work in the healthcare field is focused on improving the well-being of individuals and communities, ensuring they receive the necessary care and support for a healthy and fulfilling life.
Sources:
Featured Blogs



