Understanding and Managing Rosacea: Symptoms, Triggers, Prevention, and Treatment Options

Medically Reviewed by Dr. Rosmy Barrios - July 29, 2024
Rosacea is a complex inflammatory skin disease that still puzzles scientists. It is characterized by redness of the face that worsens with time, eventually leading to the appearance of spider veins, pimples, and bumps. Once confused for Acne Vulgaris, it is now recognized as a standalone condition. Individuals with Rosacea are susceptible to inflammatory “flare-ups” triggered by a variety of dietary, environmental, and emotional factors.[1]
The following article aims to assist those with Rosacea in managing their symptoms and avoiding flare-ups. Triggers, possible causes, prevention, and treatment options are all covered.
Symptoms and Types
Globally, Rosacea affects about 5% of the population, with a higher prevalence in those with lighter skin. The condition may affect men more severely and be underdiagnosed in those with darker skin. Although it can affect individuals of any age, symptoms commonly manifest in one’s 30s and 40s.[2]
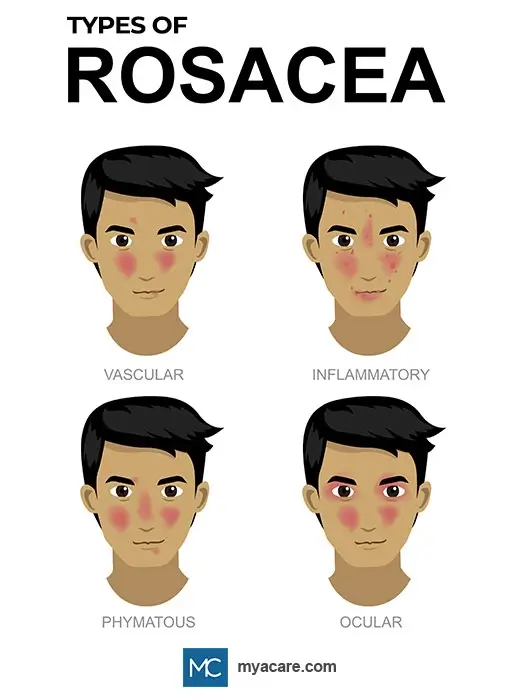
There are four types of Rosacea, each with unique symptoms as described below:
- Vascular Rosacea. In this type, the face becomes red or flushed, particularly on the cheeks. The skin may also feel hot, dry, burned, irritated, or painful. Spider veins (telangiectasia) may develop over time after repeat flare-ups and are more common in older individuals.
- Inflammatory Rosacea. Alongside redness, dryness, and irritation, the skin presents with pustules (non-acne pimples) and papules (red bumps). Swelling may also be present.
- Phymatous Rosacea. This is an advanced form of Rosacea characterized by an enlarged nose with benign growths that typically affect males.
- Ocular Rosacea. The eyes and eyelids look red, inflamed and swollen. Stye-like growths can develop on the eyelids, and the eyes may become bloodshot.
Those with Rosacea can exhibit more than one type with overlapping symptoms of varying intensity. It is vital to consult with a healthcare professional to get an accurate diagnosis, as Rosacea can be mistaken for other skin conditions.
Does Rosacea Go Away?
Some individuals with Rosacea only experience symptoms during flare-ups. Flare-ups exacerbate the symptoms, which may otherwise be mild or entirely lacking. After many years of repeated flare-ups, the skin may acquire permanent features of Rosacea, such as spider veins or redness. Men with Rosacea may develop an enlarged nose with growths.
Diseases Associated with Rosacea
Studies suggest that while Rosacea is relatively benign, flare-ups and untreated symptoms may increase the risk of other inflammatory conditions. Diseases associated with Rosacea include Diabetes, cardiovascular conditions, Rheumatoid Arthritis, Psoriasis, Alzheimer’s disease, Crohn’s disease, and chronic headaches or migraines.
Causes
Although Rosacea's underlying cause is yet unknown, experts currently believe it to be a vascular condition caused by inflammation of the skin’s blood vessels. Genetics may predispose individuals to Rosacea, yet no specific causal genes have been identified to date.
The condition can intensify when the individual is exposed to inflammatory factors, which can provoke an acute flare-up or contribute chronically towards facial redness and other symptoms. These factors are interindividual and may not be the same across all cases. Inflammatory diseases or autoimmune conditions may elevate the risk of flare-ups.
Rosacea may be caused by a weak immune system, although results are inconclusive. Patients with Rosacea are noted to have a higher amount of skin mites that naturally inhabit the pores, even in healthy individuals. The mites provoke inflammatory skin reactions due to abnormal immune responses. Evidence supports that people with Rosacea may have weakened skin immune defenses due to disruptions in the gut microbiome..[3]
Rosacea Triggers
The biggest trigger for Rosacea pertains to any factor that might increase vascular inflammation in the skin.
Common triggers for Rosacea flare-ups include:
- Excess sun exposure or sunburn
- Extreme heat or cold
- Mental-emotional stress
- Infections
- Skin mites or acne
- Spicy foods, allergies, or food sensitivities
- Harsh detergents or chemical exposures
- Intensive physical exertion
- Medications and supplements, including heart medications and Niacin
It is advisable to avoid potential triggers and causes of Rosacea flare-ups and treat symptoms where possible. A physician can help to identify unique triggers and prescribe necessary medications to manage acute symptoms.
How to Manage Rosacea and Prevent Flare-ups
The best way to manage Rosacea flare-ups is to avoid potential triggers, keep the skin clean, treat infections, and maintain a strong immune system.
The below tips can minimize flare-ups and lessen their intensity:
Embracing a Healthy Lifestyle
A nutritious diet and regular exercise can considerably aid with symptom control. These are required to support the gut microbiome, regulate inflammation and promote balanced immune activity, which reduces symptom severity and prevents potential triggers, such as infection. A healthy lifestyle can also reduce stress and contribute to emotional stability.
Working Out Personal Triggers
Since triggers differ among individuals with Rosacea, keeping a journal can help to identify and keep track of personal triggers.
Using An Elimination Journal. An elimination journal is used to record pertinent health information so that triggers or sensitivities can be identified. Daily dietary factors, physical activities, and emotional stressors ought to be taken into account. It helps to keep tabs on the time these take place as well. Eventually, patterns emerge that coincide with flare-ups, and these can be investigated more thoroughly until the source of the trigger has been found. If a trigger cannot be removed, you may be able to minimize other contributing factors until you achieve a tolerable baseline.
Perfecting a Skincare Routine for Rosacea
Skincare should be prioritized to avoid infections and to keep the skin in good health. Before designing a skincare routine for Rosacea, the following points need to be taken into consideration:
Opt for Gentle Cosmetics. If you have Rosacea, it is recommended to wash your face with gentle products free of harsh chemical additives and fragrances. Never use ordinary hand soap, astringents, or toners to wash your face. Mild products designed for Rosacea or sensitive skin are a good place to start. These may also contain active ingredients that treat Rosacea, such as sulfur.
Rosacea-Friendly Cleansers and Moisturisers. Studies have proven that those with Rosacea benefit from using products that support skin hydration and do not strip the skin of proteins or lipids. These trap moisture in the skin and lower symptoms of dryness, burning and irritation. Gentle moisturizers and cleansers that are not too astringent, cooling or alkaline can help to contain symptoms.[4]
Avoid Ingredients that Cause Flare-ups. Common ingredients known to trigger a Rosacea flare-up include menthol, capsaicin, camphor, or sodium lauryl sulfate. Natural cosmetics are not necessarily safer or more effective for those with Rosacea.
Patch Test New Products. It is important to patch-test a product on the skin, even if the product is made for those with Rosacea. Excessive activation of skin receptors can trigger flare-ups, including receptors that detect heat, cold, chemicals, or pain.[5] If a cosmetic product causes the skin to burn, or feel heated or cold when applied to a small area of the skin, it should not be part of an anti-Rosacea skincare routine.
If uncertain, consult a dermatologist to discuss which products are safe for sensitive skin prone to flare-ups.
Keeping a Constant Temperature
As explained above, excessive activation of skin receptors that detect heat, cold, or pain are capable of causing Rosacea flare-ups. Therefore, it is important for those with the condition to maintain a stable temperature at all times.
Try to Maintain a Balanced Body Temperature. Dressing in layers, sitting away from heat sources, keeping well hydrated, and ensuring that showers and baths are not too hot are practical approaches for keeping one’s body temperature balanced. If sweating on a hot day, keep a spare change of clothing nearby.
Plan for Any Weather. Protecting the skin from extreme temperature fluctuations, sun, and wind is essential. Use sunscreen with adequate SPF and sun hats during summer and be mindful of excessive sun exposure. It can be helpful to carry a scarf, windbreaker, or other jacket that covers up the face and protects it from the wind.
Being Mindful of Food and Drinks. The temperature of food or drinks can have an impact on overall body temperature, and this can contribute to triggering Rosacea symptoms. Make sure all food consumed is at room temperature or that the temperature difference is not extreme. Some individuals find that consuming only cold beverages works better for keeping flare-ups at bay.
Keeping Cool When Working Out. To avoid risking a flare-up, it is important to exercise regularly and avoid overheating while doing so. Exercising in a pool or a cooler environment is ideal. It may be a good idea to have cold water on hand or a wet cooling shirt, yet these should not be cold enough to shock the system. Palm cooling may be a useful technique for those who are very sensitive.
Stress Management and Psychosocial Support
Across studies, up to 79% of patients experience flare-ups due to emotional stress, and up to 69% suffer stress-related flare-ups at least once per month. Most of these episodes can be avoided with efforts to manage stress and keep one’s mood stable.[6]
Being Mindful of Stress. Stress is regulated by many factors, some of which are personal. Triggers of stress should be noted when attempting to find potential causes for flare-ups, as these may overlap. When stressed, it is important to disengage from it by taking a moment to breathe, taking a break, or doing something to change one’s perspective of the situation.
Stress-Lowering Activities. Socializing, exercising, and taking time out each day for oneself are all known to help ease tension and promote better stress resilience. These could well be priceless therapeutics for those with Rosacea.
Psychosocial Support. While Rosacea is made worse with emotional stress, it can also trigger it. Research shows that those with the condition are prone to being anxious and depressed more on average and that they may shy away from social interaction due to their appearance. Through passive social support and acceptance, friends and family are indispensable for helping patients cope emotionally with Rosacea and reducing stress.
Contacting a Mental Health Professional. If psychosocial symptoms persist, it is important for the patient to seek help from a mental health professional. Pharmacologic assistance is shown to be beneficial for some patients.[7]
Treatment Options
Besides looking after your skin and your health, there are several short and long-term treatment options available for minimizing Rosacea symptoms. A few of these are discussed below:
Prescription Medications. An anti-inflammatory topical or oral antibiotic may be prescribed by a dermatologist that aims to reduce the skin’s redness and control potential infections. You may be able to find topical over-the-counter medications such as Azelaic acid or sulfur ointments that can help as well. These may take several weeks before showing signs of improvement.[8]
Intense Pulsed Light Therapy. One drawback of medications is that they need to be frequently applied, or the results diminish within a matter of hours to weeks. Those with Rosacea may benefit from long-term symptom relief when opting for light therapy. Intense Pulsed Light (IPL) therapy can improve symptoms in most cases, lowering irritation, burning, and redness[9]. The results are cited to last for 6 -12 months after 3-4 sessions.
Laser Therapy. For those wanting a more permanent solution, laser therapy might be an option. In terms of getting rid of skin flushing, its efficacy is comparable to that of IPL[10]. It is a superior option for those wanting a long-term solution and who wish to address spider veins, thickened skin, or excess tissue growth. After several sessions, intensive lasers can melt away thickened skin and spider veins, causing redness and skin bumps to vanish. This treatment lasts for 3-5 years, although it requires a recovery period in which the skin is sensitive to light.
When to See a Dermatologist
It is crucial to see a dermatologist the moment a skin condition is suspected. Rosacea can be correctly diagnosed by a dermatologist, who usually recommends strategies to avoid flare-ups. They may also prescribe or suggest medications to control the initial complaint.
If symptoms get worse or occur frequently despite your best attempts at managing the condition, it is best to book a follow-up appointment and have your dermatologist check your skincare routine. If you are battling to keep tabs on personal triggers, the dermatologist can also help you better identify them. You can prepare in advance with an elimination journal and by creating a list of questions based on your observations.
Conclusion
When dealing with Rosacea, it is important to understand the symptoms and to keep track of any factors that might trigger flare-ups. Keeping Rosacea under control diminishes unwanted symptoms and may lower the potential risks of acquiring associated lifestyle diseases. Avoiding common triggers, keeping the skin clean, leading a healthy lifestyle, and coping with stress are important aspects of prevention.
It is essential to consult a dermatologist when symptoms get worse and get a proper prescription. Laser or light therapy may be an effective long-term solution.
To search for the best health providers for dermatology in Croatia, Germany, Greece, Italy, Malaysia, Singapore, Slovakia Spain, Thailand, The UAE, the UK, and the US, please use our free search engine.
To search for the best healthcare providers worldwide, please use the Mya Care search engine.
The Mya Care Editorial Team comprises medical doctors and qualified professionals with a background in healthcare, dedicated to delivering trustworthy, evidence-based health content.
Our team draws on authoritative sources, including systematic reviews published in top-tier medical journals, the latest academic and professional books by renowned experts, and official guidelines from authoritative global health organizations. This rigorous process ensures every article reflects current medical standards and is regularly updated to include the latest healthcare insights.

Dr. Rosmy Barrios is an aesthetic medicine specialist with international work experience. She earned her physician diploma at the Universidad Del Norte’s School of Medicine in Barranquilla, Colombia, and her specialty at John F. Kennedy University in Buenos Aires, Argentina. Dr. Barrios is a member of the Pan-American Aesthetic Medicine Association (PASAM) and the Union Internationale de Médecine Esthétique (UIME). She is an expert health writer with keen interests in aesthetic medicine, regenerative aesthetics, anti-aging, fitness, and nutrition. Currently, Dr. Barrios heads the Regenerative Aesthetics department at a renowned Internal Medicine clinic based in Belgrade, Serbia.
Featured Blogs



