What Is Polyneuropathy?

Polyneuropathy occurs when the peripheral nerves get damaged or diseased. The peripheral nerves make an intricate network that connects the brain and the spinal cord with the rest of the body. They serve as a two-way communication channel between the central nervous system and the body parts such as muscles, skin, and internal organs. For example, if you step on a hot surface, the peripheral nerves tell the central nervous system (brain and the spinal cord) that the feet are burning. They then carry signals back from the central nervous system to the muscles that tell them to contract to remove your feet from the hot surface.
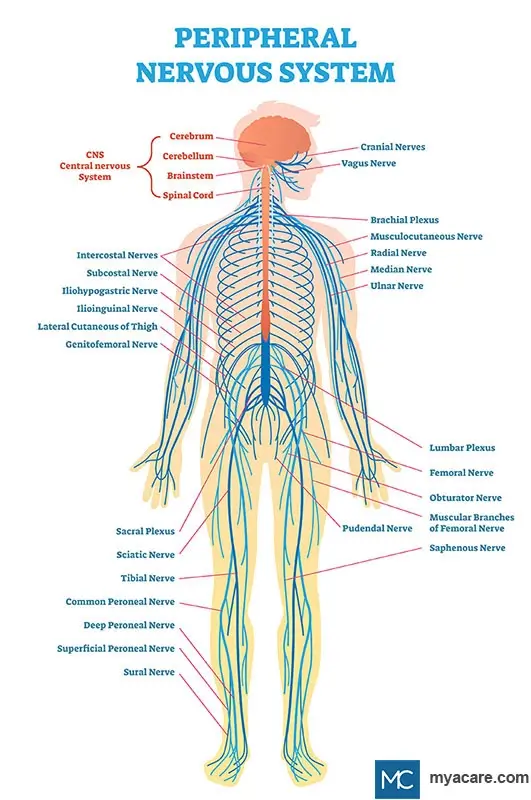
Similarly, the peripheral nerves help the brain, and the spinal cord control our bodily functions, such as our heart and blood vessels, digestion, urination, sexual function, bones, and the immune system. Damage to these nerves interrupts communication between the brain and the other parts of the body. It can impair muscle movement, prevent normal sensation in the arms and legs, and cause pain.
Hundreds of peripheral neuropathies have been identified in humans—the symptoms and prognosis depend on the damaged type of nerve. Broadly, there are three types of nerves in the body. 1) Motor nerves: control the movement of muscles; 2) Sensory nerves: inform the brain and the spinal cord about the feelings of touch, temperature, pain, pressure, etc.; 3) Autonomic nerves: control the activity of internal organs such as heart, lungs, digestive system, etc. Most neuropathies affect all three types of nerve fibers to varying degrees.
What Causes Polyneuropathy
The peripheral nerves are prone to various toxic, inflammatory, hereditary, and infectious factors that impair their health and function. Generally, polyneuropathy can be caused by the following:
- Diabetes
- Injury to the nerve from accidents falls, and sports
- Autoimmune disorders such as Guillain-Barré syndrome, Sjögren's syndrome, lupus, and rheumatoid arthritis
- Infection with viruses such as human immunodeficiency virus, varicella-zoster (chickenpox) virus, West Nile virus, cytomegalovirus, and herpes simplex virus
- High blood pressure
- High cholesterol
- End-stage kidney disease
- Amyloidosis
- Hypothyroidism
- Vitamin B12 deficiency
- Lyme disease
- Tumors
- Toxicity due to chemotherapy, alcohol abuse, and heavy metals
- Genetic factors
Symptoms of Polyneuropathy
Symptoms of polyneuropathy can vary anywhere from mild to disabling, and rarely, they may be life-threatening. The signs that an individual experience depends on the type of nerves that have been damaged. The most common symptoms of polyneuropathy include:
- Muscle weakness
- Painful cramps in the muscles
- Uncontrolled twitching in the muscles
- Problems with processing sensations such as pressure, vibrations, and temperature in hands and feet leading to numbness, tickling, and pain
- Feeling severe pain from a light touch (allodynia)
- Severe pain in the night disrupting sleep
- Problem with walking and coordination
- Excess sweating
- Heat intolerance
- Problems with eating, swallowing, digestion, and bowel movements
- Problem with urination and bladder control
- Sexual dysfunction
How is Polyneuropathy Diagnosed?
Diagnosis of polyneuropathy is often complicated and tedious as the disease is highly variable in the symptoms an individual can experience. Generally, a healthcare provider makes the first assessment of polyneuropathy based on the patient's medical history and physical exam. Blood tests are usually performed to identify conditions such as diabetes, chronic kidney diseases, infections, and other nerve damage triggers. Imaging tests such as magnetic resonance imaging and computed tomography scans are then ordered to visualize compressed nerves, tumors, bone, and blood vessel irregularities that cause polyneuropathy. Genetic testing is also an option to rule out inherited polyneuropathy.
Electrodiagnostic assessment is done by a nerve specialist to specifically find out the nerves and the muscles that have been affected by the neuropathic condition. Such a review can also provide information on the severity of the nerve damage. Electrodiagnostic assessment involves the following tests:
Nerve conduction test: This test measures the speed with which the nerves transmit the signals. The strength of the transmitting signal is also evaluated. During this test, small electric patches are placed on the patient's skin (covering specific nerves and muscles) on different limbs. A brief pulse of electricity is then applied to the patch.
Needle electromyography: A thin needle is inserted through the skin into the specific muscle in this test. The movement of the muscle and its electrical activity is then evaluated. Such examination can tell if the damage is in the muscle or the underlying nerve.
Along with these tests, a healthcare provider may also do a skin biopsy to evaluate any dysfunction in the tiny nerves present underneath the skin. Autonomic testing to measure the ability to sweat and sensory testing to measure the degree of loss of sensations like touch and temperature are some of the other tests that provide valuable information.
Available Treatment Options for Polyneuropathy
There are two distinct aspects to the treatment of polyneuropathy. If a treatable condition causes neuropathy, managing it might reverse or worsen it. If the underlying cause of polyneuropathy can’t be treated, the goal is to manage the symptoms and improve the quality of life. The treatment options include the following:
- Improving nerve health by adopting a healthy lifestyle. Lifestyle adaptations to include a balanced diet, maintaining optimal weight, managing diabetes and high blood pressure through exercise, limiting alcohol, and correcting vitamin deficiency may benefit the nerves.
- Physical therapy and complementary techniques such as massage and acupuncture may also help alleviate the symptoms of polyneuropathy.
- Using mechanical aids such as braces for hands and feet may help in reducing the physical disability.
- Using immunosuppressive drugs to suppress abnormal activity in the immune system leading to nerve damage.
- Pain management can be done using pain medication, local anesthetics, lidocaine patches, or opioids. Sometimes, antidepressants are also recommended for managing chronic pain occurring due to polyneuropathy. Such medicines can increase the brain’s ability to inhibit the pain signals transmitted continuously through damaged nerves.
- Surgery is recommended treatment for some types of polyneuropathies (polyneuropathy caused by displaced discs in the back). However, sometimes surgical intervention is contraindicated as it might worsen the pain symptoms.
- More sophisticated and less damaging procedures such as transcutaneous electrical nerve stimulation (TENS) have been recommended mainly over surgeries. TENS is a non-invasive procedure that involves attaching electrodes to the skin at the site of pain and applying a gentle electric current.
Conclusion
Polyneuropathy is a debilitating condition caused by the simultaneous malfunction of many peripheral nerves of the body. A timely diagnosis of the cause of polyneuropathy is the only way to prevent the disease from disrupting a patient’s life.
To search for the best Neurology Healthcare Providers in Croatia, Germany, India, Malaysia, Spain, Thailand, Turkey, Ukraine, the UAE, UK and the USA, please use the Mya Care search engine.
To search for the best healthcare providers worldwide, please use the Mya Care search engine.
Dr. Vedangana Saini has a Ph.D. in Neuroscience. She has done multiple postdoctoral fellowships from the University of Nebraska Medical Center, Omaha, and Weill Cornell Medicine, New York. Currently, she is working as a freelance scientific writer with a mission to educate the lay public about recent scientific and medical developments. Dr. Saini has written extensively on healthcare, neuroscience, and mental health. She holds several publications in peer-reviewed journals in the form of research papers, review articles, and book chapters.
References:
Featured Blogs



