What Is Giant Cell Arteritis?
Causes of Giant Cell Arteritis
Blood Vessels Impacted by Giant Cell Arteritis
Giant cell arteritis is an inflammatory condition that affects certain large blood vessels. This is also known as temporal arteritis as the inflammation commonly impacts the head arteries as well. The condition is named after the giant immune cells that are found in inflamed blood vessels.
Causes of Giant Cell Arteritis
Giant cell arteritis is a vasculitis that specifically affects arteries of the body that contain a lot of elastic connective tissue. The cause of this arteritis is an inflammatory reaction in which the specific blood vessels are damaged by an autoimmune reaction. This is similar to other types of vasculitis such as Takayasu’s arteritis.
Blood Vessels Impacted by Giant Cell Arteritis
The blood vessels of the cardiovascular system that are most affected by giant cell arteritis include:
- Carotid and temporal arteries: The carotid arteries occur in the neck and travel into the head. Temporal arteries branch off the carotids and are found in the temporal part of the skull.
- Coronary arteries: These arteries occur on the surface of the heart itself and supply blood to the heart tissue.
- Cranial arteries: These are arteries of the brain.
- Aorta: This is the main artery of the body that leaves the left side of the heart and branches into all the other arteries of the body. It is also the largest artery of the body.
Symptoms of giant cell arteritis
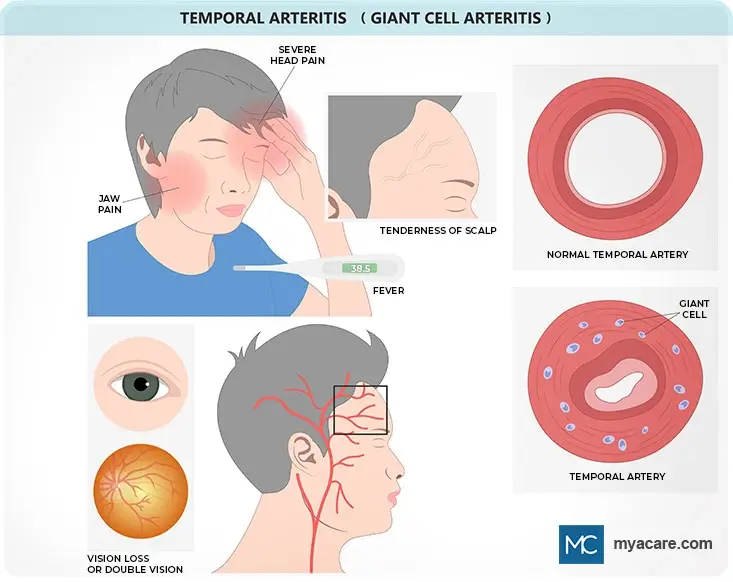
There are several symptoms that a person can have which can suggest giant cell arteritis. These symptoms are listed and discussed below.
- Fatigue: A person feeling more tired than usual may have some inflammatory condition such as temporal arteritis.
- Low-grade fever: This is when body temperature is slightly elevated, in other words not higher than 100.4oF (38oC).
- Night sweats: These are a less familiar symptom of giant cell arteritis.
- Weight loss: A person with any type of vasculitis can lose weight because they lose their appetite. This is also the situation with temporal arteritis.
- Headache: This is when there is throbbing pain in the head but particularly over the temples, however, the tenderness can spread to other parts of the head. A headache in people over 50 is a potential sign of arteritis, but other conditions need to be ruled out.
- Vision problems: Several problems with the eyes can occur including ptosis, diplopia, vision loss in one or both eyes, and scotoma.
- Dizziness: Compromised blood flow in the brain due to arteritis can cause dizziness.
- Jaw pain: A pain in the jaw is one potential sign of arteritis.
- Tongue pain: The tongue may hurt because of cranial nerve inflammation due to arteritis.
- Transient ischemic attacks: These are called TIAs. The patient has stroke-like symptoms that do go away; however, a TIA is often a precursor to a stroke.
- Thoracic or abdominal aorta aneurysm: An aneurysm is when there is a bulge in a blood vessel, in this case, the thoracic or abdominal aorta enlarges. An aneurysm is a dangerous condition because a dissection can occur, which can be fatal. Aortic aneurysms are often seen in the late stages of giant cell arteritis.
Complications of Giant Cell Arteritis
The inner wall of blood vessels can become so severely damaged by giant cell arteritis that the result is ischemia (lack of oxygen). This ischemic damage and damage due to excessive inflammation can lead to further complications. Complications of giant cell arteritis can be life-changing. Such complications include:
- Vision loss: Permanent loss of sight occurs in about 30% of patients with arteritis who have eye problems due to the condition.
- Aneurysm dissection: Many aortic dissections result in death; rapid treatment is needed.
- Stroke: A stroke due to giant cell arteritis can lead to permanent damage to the nervous system and even death.
Giant Cell Arteritis Risk Factors and Comorbidities
Giant cell arteritis is often found along with another condition, polymyalgia rheumatica (PMR). PMR is also an inflammatory problem in which the muscles of certain parts of the body are inflamed. Risk factors for giant cell arteritis include the following:
- Having PMR
- Being 50 years or older
- Being female
- Having Scandinavian or other North European ancestries
Diagnosis of Giant Cell Arteritis
A series of tests can be done to diagnose giant cell arteritis. These are described below.
- Complete blood cell count: This is called a CBC and can show that a person has mild anemia (which is possible in giant cell arteritis).
- C-reactive protein: This is a common marker indicating that there is inflammation in the body. A C-reactive protein (CRP) value of more than 2.45 mg/dL may indicate giant cell arteritis.
- Erythrocyte sedimentation rate (ESR): An ESR of more than 50 mm/h may suggest arteritis.
- Imaging tests: Doppler ultrasounds and MRI tests can show problems with blood flow through arteries and the presence of any aneurysms. It is not a conclusive test for arteritis though.
- Biopsy: A small section of the temporal artery can be biopsied and examined for signs of inflammation. The presence of giant multinucleated cells and monocytes collecting in the artery is a sign of the condition. The biopsy is considered the most conclusive way to diagnose the condition.
Treatment of Giant Cell Arteritis
Treatment methods include medications that are discussed below.
- Corticosteroids: These should be given as soon as the illness is suspected. IV methylprednisolone or oral prednisone can be given. The use of such corticosteroid medicine is important in helping prevent vision loss due to arteritis.
- IL-6 receptor antagonist: The medication Tocilizumab is sometimes helpful but cannot be given to people who have diverticulitis. Tocilizumab is occasionally combined with corticosteroids.
- Aspirin: Only a low dose (not more than 150mg) per day should be taken by patients. Aspirin is an anti-inflammatory and also helps stop blood clots from forming. Check with your doctor first before taking aspirin or any new medication.
Adopting a healthy lifestyle by following a balanced healthy diet and exercising regularly are recommended if you have temporal arteritis. This will not reverse the arteritis but it can help you feel better and may help prevent other illnesses that could worsen your general state of health.
Conclusions
Giant cell arteritis is not that common, occurring in about 10 people out of every 100,000 people. However, it can have dangerous complications and can cause death. Death rates are 2% for individuals who are diagnosed with the condition. Correct diagnosis and rapid treatment of giant cell arteritis are needed to prevent complications.
To search for the best Neurology Healthcare Providers in Croatia, Germany, India, Malaysia, Spain, Thailand, Turkey, Ukraine, the UAE, UK and the USA, please use the Mya Care search engine.
To search for the best healthcare providers worldwide, please use the Mya Care search engine.

Dr. Rae Osborn has a Ph.D. in Biology from the University of Texas at Arlington. She was a tenured Associate Professor of Biology at Northwestern State University, where she taught many courses to Pre-nursing and Pre-medical students. She has written extensively on medical conditions and healthy lifestyle topics, including nutrition. She is from South Africa but lived and taught in the United States for 18 years.
Sources
Featured Blogs



